Advanced Endoscopy Procedures: EMR, ESD and Other Endoscopic Treatment Techniques
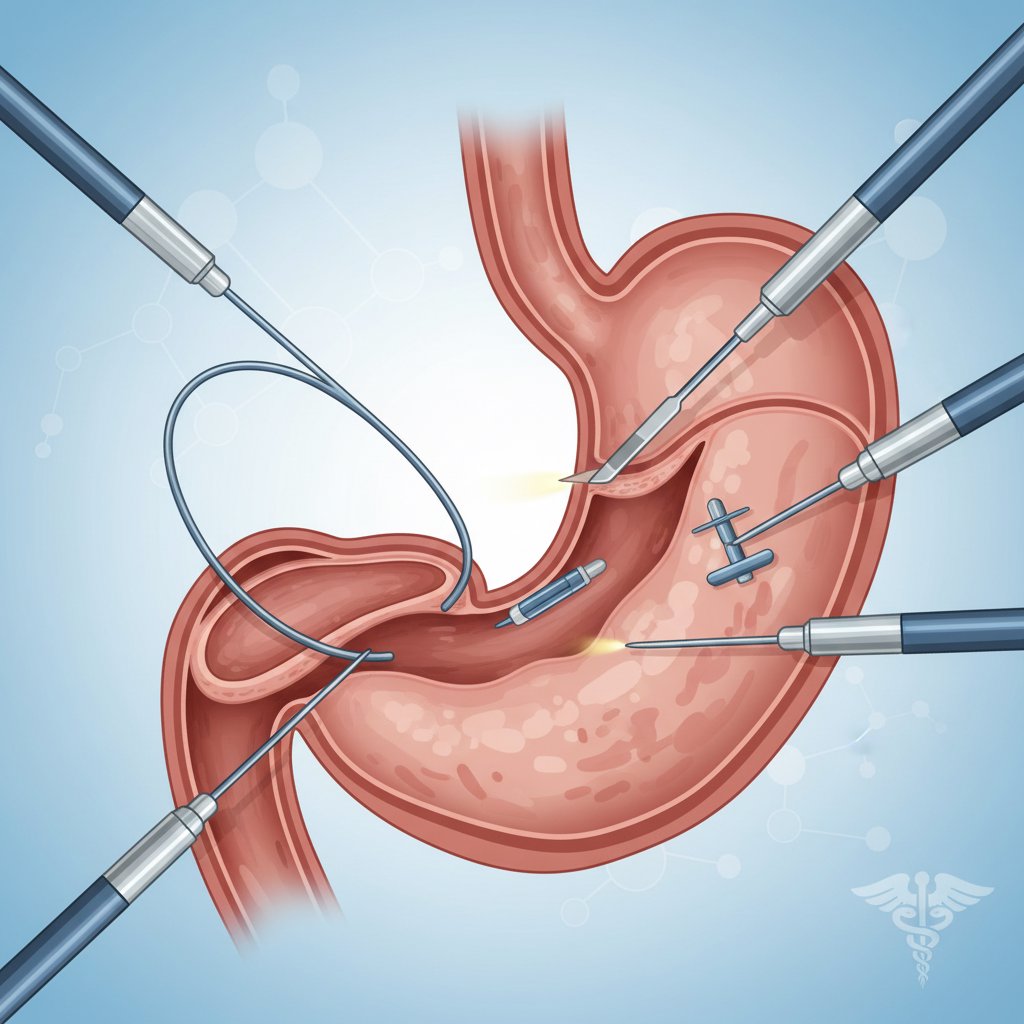
Advanced endoscopy encompasses advanced procedures that aim not only to diagnose but also to remove or control the lesion by performing endoscopic treatment in the same session in appropriate patients. Polyps detected during colonoscopy and gastroscopy may not always be safely removed by “standard” methods. More advanced techniques are needed in cases where the polyp is broad-based, spreads on the surface, has been previously intervened and scarring has occurred, or is suspected of early cancer. At this point, methods such as EMR (endoscopic mucosal resection) and ESD (endoscopic submucosal dissection) come into play.
In this article, we will answer the most frequently asked questions such as “What is EMR?”, “What is ESD?”, “What is the difference between EMR and ESD?” in a patient-friendly language. We will also detail the differences between endoscopic polyp removal and EMR/ESD, what to consider in pre-procedure preparation (especially blood thinners), possible risks and post-procedure follow-up. Finally, we will add a brief guide to other endoscopic surgery and advanced endoscopy techniques other than EMR/ESD.
Note: This content is for general information purposes; consult your gastroenterologist for a personalized treatment plan.
What is advanced endoscopy? How is it different from conventional endoscopy?
Advanced endoscopy goes beyond the “diagnostic” use of classical endoscopic examinations such as gastroscopy and colonoscopy. The aim is not only to see the lesion, but also to remove the lesion with an endoscope in the appropriate patient, both to treat it and to provide sufficient material for pathologic evaluation. This approach can also be referred to as “endoscopic surgery” as it can offer the chance of treatment without the need for open/close surgery in many cases. However, there is an important nuance here: Endoscopic procedures are not always “substitutes for surgery”; in some patients they may be an alternative to surgery, while in others they are planned as a bridge or complementary step to surgery.
Classical endoscopic polyp removal (standard polypectomy) is usually sufficient for small, stalked polyps. But some lesions are more complex:
- Can be wide-based or flat
- Can spread on the surface (laterally spreading tumor)
- Previous partial removal and scarring may have developed
- Vascular structure and surface pattern may be suspicious for early cancer
In such cases, advanced techniques such as EMR/ESD provide more controlled removal of the lesion and more accurate evaluation of the borders. In addition, advanced clip systems (such as OTSC) for bleeding control, stent applications in stenosis, ablation methods in cases such as Barrett’s esophagus are also included in the scope of advanced endoscopy.
Internal links for more basic content:
What is EMR (Endoscopic Mucosal Resection)? In which cases is it preferred?
**What is EMR? EMR (Endoscopic Mucosal Resection) is the endoscopic removal of lesions in the mucosa, the most superficial layer of the digestive tract wall. EMR is an effective endoscopic treatment method in selected lesions in many regions, especially in the colon and stomach. it can be considered as a bridge between “standard polypectomy” and “advanced endoscopic resection”.
How to do EMR (in patient language)
The basic rationale of EMR is to separate the lesion from the underlying tissue and remove it more safely. Therefore, in most cases, “lifting” is achieved by injecting fluid under the lesion. When the lesion rises, it is grasped with a snare (lasso) and removed in a controlled manner. Clips may then be applied in some patients to reduce the risk of bleeding. This approach makes endoscopic polyp removal safer and “controlled”, especially in appropriate lesions.
What does en bloc vs piecemeal mean?
- En bloc resection: It is a single piece removal of the lesion. For pathology, the margins are more clearly assessed.
- Piecemeal resection: Removal of the lesion piece by piece. It may be required more frequently with EMR in large lesions. The risk of recurrence is monitored more closely during follow-up.
These concepts are also important in the interpretation of phrases such as “R0 resection” that you may encounter in the pathology report. (R0 generally means that no tumor/lesion is seen at the margins of the removed fragment; nevertheless, the clinical decision is based on the complete pathology report)
###Who is EMR performed? the answer to the question “Who should undergo EMR?” depends on the size, shape, location, surface characteristics and experience of the physician. In general, EMR is considered for superficially located lesions that can be safely removed with an endoscope. In some patients, EMR may be the most appropriate option before surgery; in others, additional treatment may be planned according to the pathology result.
Related content suggestion: What should be considered after endoscopic polyp removal?
What is ESD (Endoscopic Submucosal Dissection)? Why is it a more advanced technique?
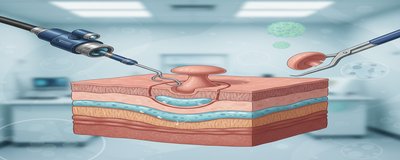
**What is ESD? ESD (Endoscopic Submucosal Dissection) is an advanced method in which special endoscopic blades are used to dissect the submucosal layer beneath the lesion and the lesion is usually removed en bloc (in one piece). ESD is technically more difficult, takes longer and requires more experience than EMR, but can offer significant advantages in the right patient.
Advantages of ESD
- The probability of en bloc inference is higher: This allows a clearer answer to the question “are the margins clear?” in pathology.
- More accurate staging: The depth of the lesion and possible risk features can be better assessed.
- It may reduce surgery in selected patients: Especially in some superficial early cancer/leading lesions, endoscopic treatment may be sufficient if the criteria are appropriate.
###Who is ESD performed? the question “Who is ESD performed?” also varies on an organ basis (esophagus-stomach-colon). In general, ESD may be more appropriate for lesions that are larger, spread on the surface, have carefully defined borders and where a single piece removal is critical. In some patients, further evaluations (advanced imaging, endoscopic ultrasound, etc.) may be planned before the procedure.
Is EMR or ESD better?
there is no single answer to the question “EMR or ESD is better?”. The correct question is: “What is the goal in this lesion; safe extraction, single piece extraction, clarity of pathology margins?” The decision is therefore based on the characteristics of the lesion and the experience of the center.
The table below provides a quick summary of the EMR ESD difference:
| Criteria | EMR | ESD |
|---|---|---|
| Main goal | To remove the mucosal lesion | To remove the lesion mostly en bloc |
| Mode of inference | En bloc or piecemeal | Mostly en bloc |
| Processing time | Generally shorter | Generally longer/technical |
| Pathology evaluation | May be limited if piecemeal | Borders can be evaluated more clearly |
| Risk of recurrence | May be higher if piecemeal | May be lower in selected cases |
| Complication profile | There is a risk of bleeding/perforation | Risk profile may change with technical difficulty |
How does endoscopic polyp removal (polypectomy) differ from EMR/ESD?
“Endoscopic polyp removal” is one of the most frequently searched phrases and most often refers to a standard polypectomy performed during colonoscopy. This procedure plays a critical role in colon cancer screening. However, not all polyps are at the same risk and not all polyps can be safely removed with the same technique.
For which polyps is a standard polypectomy sufficient?
- Small and stalked polyps
- In lesions with clear borders and benign surface pattern
- In cases where the risk of bleeding/perforation is considered low
In these patients, the procedure is usually shorter and most patients can be discharged the same day (according to the physician’s plan). Nevertheless, it is important to follow the post-procedure recommendations as even “small polyps” can sometimes carry a risk of bleeding.
When is advanced endoscopy needed?
In the following cases, advanced endoscopic treatment methods such as EMR/ESD may be considered:
- If the polyp is broad-based or flat
- If it spreads on the surface
- Previous partial removal and scarring
- If there are suspicious endoscopic findings for early cancer
- If one-piece extraction seems critical in terms of pathology
Therefore, “colon polyp removal” is not always a single type of procedure; sometimes standard polypectomy, sometimes EMR, sometimes ESD is required.
Related internal link: Colon cancer screening and polyps
Other advanced endoscopic techniques (options other than EMR/ESD)
Advanced endoscopy is not just about EMR and ESD. Today, many problems can be managed with endoscopic surgical approaches in appropriate patients. Here are some common techniques:
- EFTR (Endoscopic Full-thickness Resection): Allows full-thickness removal of the digestive wall in selected lesions. It may be considered especially in scarred lesions or lesions difficult to classical EMR/ESD.
- POEM: It is a treatment approach through an endoscopic tunnel in motility disorders that cause swallowing difficulties such as achalasia.
- RFA (Radiofrequency Ablation): In cases such as Barrett’s esophagus, it can be used for ablation of abnormal tissue in appropriate patients.
- APC (Argon Plasma Coagulation): It can be applied for coagulation/ablation in superficial bleeding foci or some superficial lesions.
- Endoscopic clips/OTSC: can be used for bleeding control after EMR/ESD, closure of some small perforations or reinforcement of high-risk areas.
- Endoscopic stent: May be preferred for opening of stenoses, management of some leaks or symptom control in tumor-induced obstructions.
Which of these techniques is appropriate is determined by the location and size of the lesion, suspicion of pathology, the patient’s comorbidities and the experience of the center. When choosing a center, it may be useful to ask about criteria such as “annual number of cases”, “complication management” and “pathology support”.
Pre-procedure preparation, risks and post-procedure follow-up (practical guide)
Success in advanced endoscopy procedures is not limited to technique. Preparation, medication management and follow-up planning are as important as the procedure.
Pre-procedure preparation: Most frequently asked questions
- Fasting: Fasting for a certain number of hours is usually required for upper digestive system procedures.
- Bowel cleansing: Bowel preparation determines the image quality in colon procedures (colonoscopy, EMR/ESD). Inadequate preparation may lead to the lesion being missed or the procedure being delayed.
- Blood thinners and other medications: Queries such as “blood thinners before polyp removal”, “aspirin before colonoscopy polyp removal” are very common. However, the decision to stop/stop these medicines is individualized (heart stent, clot risk, arrhythmia, kidney function, etc.).
- Do not discontinue your medication on your own.
- Ask for a written plan from your team who will perform the procedure.
- Additional evaluations: Some lesions may require pre-procedural biopsy, further imaging or tests such as EUS.
Possible risks and complications
As with all endoscopic treatment procedures, there are risks in EMR/ESD:
- Bleeding: It may occur during or after the procedure. “Bleeding after polyp removal” can be seen especially in the first few days; in some cases there may be delayed bleeding.
- **Perforation: **Perforation is a rare but important risk. Some perforations can be closed with endoscopic clips; some may require surgery.
- Stenosis: Especially after large area extractions, stenosis may develop in some areas.
- Infection and pain: Although less common, it may require close follow-up after the procedure.
Which symptoms should I go to the emergency room?
Contact your healthcare provider without delay in the following cases
- Severe/increased abdominal pain
- Non-stopping or intense rectal bleeding, black stools
- High fever, chills
- Fainting, severe weakness, palpitations
- Significantly increased dysphagia after esophageal procedures
Post-procedure follow-up: Pathology and control plan
- Nutrition: The answer to the question “How should nutrition be after polyp removal?” depends on the location and extent of the procedure. The discharge instructions given to you are the most accurate source.
- Pathology result: is the most critical outcome of EMR/ESD. phrases such as “en bloc”, “piecemeal”, “R0 resection” give information about the completeness of the extraction and the cleanliness of the margins.
- Control colonoscopy/endoscopy: The question “When is the control colonoscopy after polyp removal?” is planned according to polyp type, size, removal method and pathology. It is therefore important not to miss check-up appointments.
Short summary: What should you take away from this article?
- Advanced endoscopy is a powerful endoscopic treatment option in selected patients.
- EMR is an effective and practical method in many lesions; piecemeal removal may sometimes be required in large lesions.
- ESD is a more technical procedure, but often provides en bloc inference, enhancing pathology assessment.
- Endoscopic polyp removal is not always the same; standard polypectomy, EMR or ESD may be required depending on the characteristics of the polyp.
- Preparation, medication management and follow-up (especially pathology and follow-up endoscopy) are as important as the procedure.
Medical content trust note (E-E-A-T): To increase trust in health content, it is also beneficial for SEO if you add “author/expert approval”, “date of last update” and, if possible, a short reference section based on guidelines such as ESGE/ASGE.