Stenting of the Esophagus (Esophageal Stent): Endoscopic Stenting
Complaints such as a stuck feeling in the throat during swallowing, increasing difficulty swallowing (dysphagia), inability to swallow solid foods or chest pressure while eating can sometimes be associated with esophageal stricture or esophageal obstruction. In such cases, the main goal is to ensure that the patient can eat safely, reduce weight loss and continue the treatment plan for the underlying cause (e.g. oncologic treatments or surgical preparation) without interruption. One of the methods used for this purpose is the placement of a esophageal stent (also known as esophageal stent).
Eesophageal stenting is an endoscopic procedure that can significantly relieve swallowing in most patients. However, it is not the first choice for all swallowing problems; the cause, location, length and general health status of the patient should be evaluated. In this article, we will discuss what endoscopic stent application is, to whom it can be recommended, the pre-procedure-procedure-day-post-procedure process, nutrition after esophageal stent recommendations and warning signs such as “signs of stent slippage” in a patient-friendly language.
Note: This content is for informational purposes; gastroenterology or related surgical branch physician evaluation is required for diagnosis and treatment plan.
What is an esophageal stent and how does it work?
**An esophageal stent is a tubular device that is inserted into the esophagus to widen and keep open a narrowed area inside the esophagus. Stents are usually “self-expanding”, meaning that after being placed in the narrow area, they open and widen the esophageal canal (lumen). This facilitates the passage of food and fluids and can provide rapid symptom control as part of treatment of dysphagia.
The main purposes of use of the stent are as follows:
- Open the stenosis/obstruction: It facilitates feeding, especially in patients with significant esophageal obstruction.
- Improving quality of life: As swallowing is relieved, the patient’s oral intake may increase, which can help reduce weakness and weight loss.
- Management of a leak or fistula (in selected cases): In some cases, covered stents may be used to reduce leakage or close an abnormal passage (at the physician’s discretion).
- Being a bridge to treatment: In some patients, a stent may be a temporary solution to maintain nutrition until more extensive treatment.
Whether the stenosis is malignant (malignant) or benign (benign) is particularly important when making the stent decision. Because the goal of the stent, the duration of stay and the follow-up plan may change according to this distinction.
Content recommendation: If you want to read more about the causes of swallowing complaints: What is Dysphagia (Dysphagia)?
In which cases is it necessary to insert an esophageal stent?
**Esophageal stenting is not suitable for all patients and is often considered as part of an “outcome-oriented” treatment plan. After evaluating the degree of the complaint, the location/length of the stenosis, the underlying cause and the general condition of the patient, the physician brings up the stent option.
1) Malignant strictures (cancer-related strictures)
Esophageal cancer or tumors compressing from surrounding tissues may cause narrowing of the esophagus, leading to significant difficulty swallowing. In this group esophageal stent is usually:
- fast symptom control,
- facilitating nutrition,
- improving quality of life for the purpose of nutrition. In some patients, it may be a palliative solution to maintain nutrition while chemotherapy/radiotherapy is ongoing or planned.
2) Benign stenoses (benign stenoses)
In benign strictures, the approach is more selective. Examples
- Strictures due to ingestion of corrosive substances
- Post-surgical strictures
- Radiation stenosis
- Strictures due to long-term reflux (in selected cases)
In these patients, the first option is often endoscopic dilatation (balloon/buji dilatation). However, in recurrent or “refractory” stenoses, a stent may be considered in the appropriate patient.
3) Special conditions such as leakage/fistula
In cases of fistula between the esophagus and airways or postoperative leakage, especially capped stent options may be beneficial in some cases.
Who may not be suitable?
In cases of extremely high risk of perforation, active uncontrolled bleeding, severe general impairment or anatomical difficulties, a stent may not be appropriate. Therefore, the answer to the question “is a stent necessary?” is personalized.
Content recommendation: To understand the process: What is Endoscopy, How is it Performed?
How is endoscopic stenting performed? (Before-after procedure)
**Endoscopic stent placement is usually performed in the endoscopy unit. Although the details of the procedure may vary according to the center and the clinical condition of the patient, the general flow is as follows.
Preparation before the procedure
- Fasting: You are usually asked to fast for a certain period of time before the procedure.
- Medication regimen: Blood thinners, diabetes medications and some supplements may require physician guidance. Do not stop medication on your own.
- Evaluation: The location/length and cause of the stenosis are clarified by endoscopy and imaging if necessary.
Sedation or anesthesia?
“**Does stenting hurt?” is a common question. During the procedure, pain sensation is minimal in most patients due to sedation. However, chest pressure/pain, tenderness when swallowing or increased reflux may be observed in the first days after the procedure. These complaints are usually managed with follow-up and appropriate medication; nevertheless, in case of severe complaints, the physician should be informed.
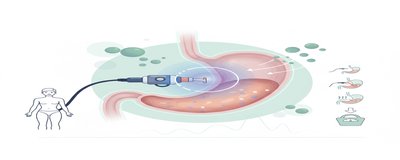
Placement of the stent
The stenosis area is visualized with an endoscope, the appropriate stent size is selected and the stent is placed in the narrow area. After the stent is deployed, passage is checked. In some cases, additional imaging may be used for position confirmation.
Post-procedure follow-up
Patient complaints (pain, nausea, swallowing) are monitored. Discharge is planned according to the patient’s general condition, comorbidities and conditions that develop during/after the procedure.
Practical information: In some patients, swallowing relief is evident on the same day, while in others, gradual improvement may be seen within a few days as the stent is fully seated and edema decreases.
Types of stents, post-stent nutrition and complications (most curious)
This chapter answers the questions “which stent to choose?” and “what to consider afterwards?” together. Because the type of stent can affect both the risk of esophageal obstruction and the follow-up plan.
Types of stents (short and clear summary)
- SEMS (self-expandable metal stent): It is one of the frequently used stent types.
- Plastic stent: May be preferred in selected cases.
- Covered stent / uncovered stent:
- Covered stents can help reduce the growth of tumor tissue into the stent and close it in cases of leakage/fistula; however, some patients may have a higher risk of stent migration (stent slippage).
- Non-coated stents may hold better, but the risk of re-narrowing with tissue growth may increase.
The physician decides which stent is appropriate based on the cause of the stenosis (malignant/benign), the location/length of the stenosis and the patient’s complaints.
Nutrition after esophageal stenting: What to eat and what to watch out for?
Nutrition after esophageal stenting is very important to improve comfort and reduce the risk of stent occlusion. Centers may have different protocols; the following recommendations provide a general framework:
- First 24 hours (frequently): Clear liquids (such as water, light tea, broth).
- The next 1-3 days: Soft/mash consistency (soup, yogurt, puree, well cooked soft foods).
- Gradual transition: Transition from soft solids to a more normal diet according to physician’s recommendation.
Golden rules
- Take small bites, chew well.
- Support each bite with water (facilitates passage through the stent).
- Be careful with foods that are too dry, hard, fibrous and tend to “stick” (e.g. very dry bread, hard pieces of meat).
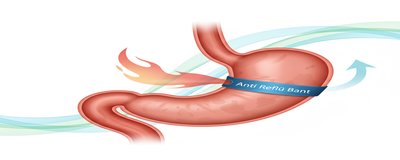
- If there is a tendency to reflux, it is important to elevate the head at bedtime, not to eat heavy meals at late hours and to use reflux medications regularly if recommended by the physician.
Content recommendation: For more general information on swallowing safety and diet: Swallowing Therapy and Nutritional Safety
Possible risks and “when to go to the emergency room?”
Common complaints:
- Pressure/pain in the chest area
- Reflux and heartburn
- Tenderness when swallowing
Complications that may be more serious:
- Stent slippage (migration)
- Stent occlusion
- Bleeding, aspiration, rarely perforation
**What are the symptoms of a slipped stent?
- Difficult swallowing again or sudden worsening
- Unexpected vomiting/burping
- Different, increasing discomfort in the chest
- Reinsertion of previously comfortable foods
**Warning signs that may require urgent evaluation
- Severe chest pain or shortness of breath
- Bloody vomiting, black feces
- High fever, chills
- Inability to swallow even saliva, rapidly increasing difficulty swallowing
In these cases, contact the emergency room or the center that performed the procedure without delay.
How long does the stent stay, is it removed? (Follow-up plan and common questions)
the answer to the question “**How long does the esophageal stent last?” is directly related to the cause of the stenosis, stent type and treatment target. For this reason, clear durations seen on the internet such as “this many days” may not be valid for every patient.
Malignant stenoses (cancer-related)
In cancer-related strictures, esophageal stent can often be used for long-term/palliative purposes. Follow-up is planned more closely if complaints return, weight loss persists, and complaints such as reflux and pain increase. In some patients, the stent may also positively affect treatment tolerance by enabling oral intake while oncologic treatments (chemotherapy/radiotherapy) are ongoing.
Benign stenosis (benign)
Since the goal in benign strictures is often “to provide a permanent patency”, some stents can be placed temporarily and removed after a certain period of time. Therefore, the answer to the question “**is the esophageal stent removed?” is “yes” in most cases; however, the removability and timing depends on the type of stent, the behavior of the stenosis and the physician’s plan.
Frequently asked questions (FAQ)
- **How many minutes does endoscopic stenting take? It depends on the case; preparation and post-procedure observation times are added. The net duration is shared by the team planning the procedure.
- **When does swallowing improve after stenting? Some patients may experience relief on the same day, while others may experience gradual improvement over several days.
- **Can the stent become blocked? Yes. Obstruction may develop especially with inappropriate foods, eating without chewing enough or with tissue growth due to underlying disease. If swallowing becomes difficult again, evaluation is required.
- **What happens if the stent migrates? Stent migration may lead to a return of swallowing complaints or other symptoms. If in doubt, contact your physician without delay.
- **Is there an option other than a stent for the treatment of dysphagia? Yes. Depending on the cause, endoscopic dilatation, drug treatments, oncologic treatments, surgical approaches or nutritional support methods may be considered.
Related content: About endoscopic dilatation of strictures: What is Endoscopic Dilation?
Final word: Choosing the right patient and good follow-up determines success
In summary, esophageal stent and endoscopic stent application is an important intervention that can rapidly reduce the complaints of difficulty in swallowing due to esophageal obstruction and facilitate feeding in appropriate patients. However, the type of stent, duration of stay, nutrition after esophageal stent plan and frequency of follow-up are individualized. Even simple measures such as eating small bites, chewing well and supporting with water after the procedure can be effective in reducing the risk of stent blockage.
If you have increasing difficulty swallowing, weight loss or warning signs such as a feeling of “re-insertion”, severe pain or bleeding after stenting, contact your healthcare provider without delay. Proper assessment and regular follow-up significantly improve both safety and quality of life.