What is an Ulcer? Gastric Ulcer and duodenal Ulcer (Peptic Ulcer) Guide
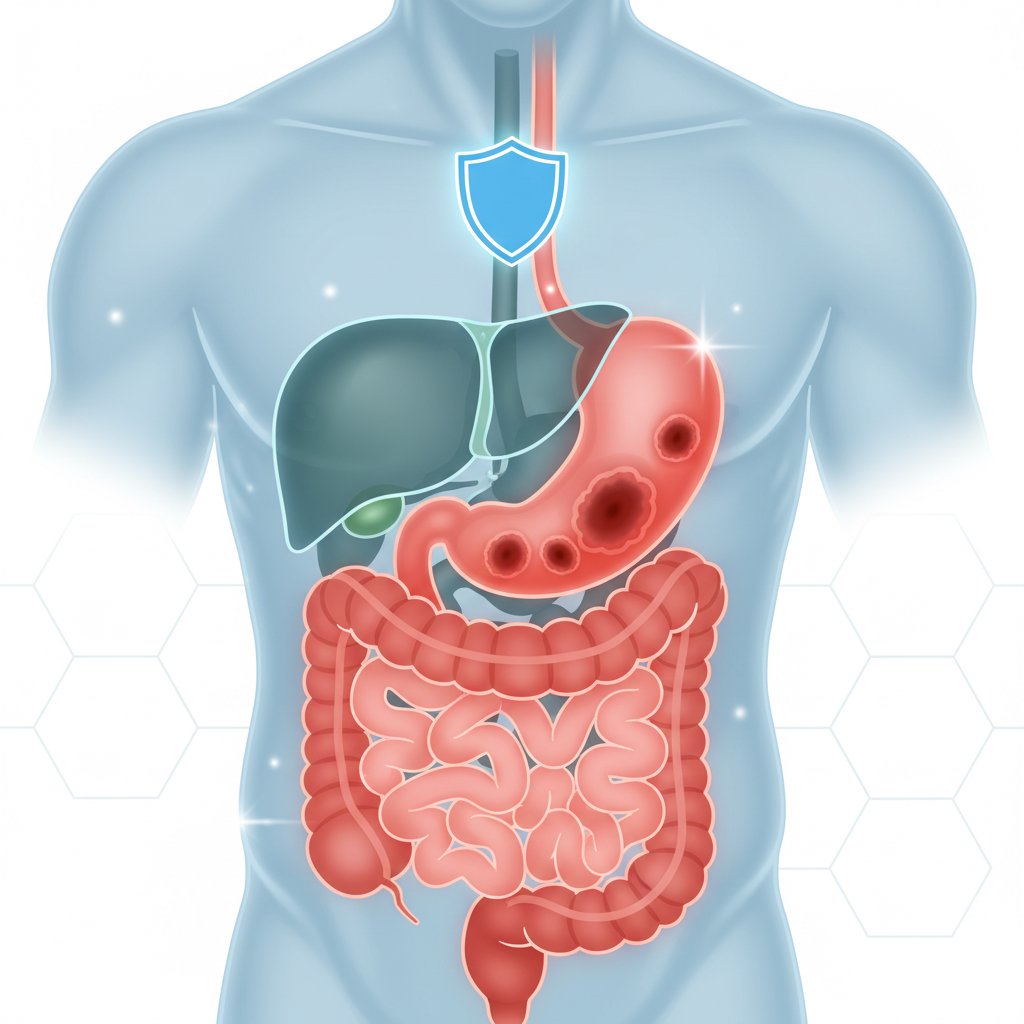
Ulcer is a common health problem that is often confused with gastritis and reflux. In its simplest definition, a peptic ulcer is a “wound” formed on the inner surface of the gastric or duodenum by the effect of stomach acid and digestive fluids. although the answer to the question “**What is an ulcer?” is so clear, the symptoms, causes and treatment of ulcers may vary from person to person.
Two most common causes stand out: Helicobacter pylori (H. pylori) infection and the use of NSAIDs/painkillers (e.g. ibuprofen, naproxen). While some people have mild symptoms, others may develop serious conditions such as ulcer bleeding. Therefore, it is important to read the symptoms correctly instead of waiting for it to “pass”.
In this article, we will discuss critical questions such as gastric ulcer, symptoms of ulcer, ulcer treatment, diagnostic methods, nutritional recommendations and “when to go to the emergency room?” in an understandable language. (For similar topics such as gastritis and reflux, you can also take a look at our articles What is Gastritis? and Reflux Symptoms)
What is an Ulcer (Peptic Ulcer)? Gastritis and its Difference with Reflux
Peptic ulcer is the weakening of the mucosa protecting the inner surface of the stomach or duodenum, causing acid and digestive enzymes to cause erosion/wound in the tissue. When this wound deepens, pain, burning, indigestion and even bleeding may occur. the most critical point for those who ask “What is an ulcer?” is this: An ulcer is more than a superficial irritation; there is an actual loss of tissue in the mucosa.
So, how to distinguish between ulcers and conditions that are often confused with ulcers?
- The difference between gastritis and ulcer: Gastritis is an inflammation of the lining of the stomach; an ulcer is a wound. Gastritis is more diffuse and sometimes more “diffuse superficial”, while ulcer is a more “focal” lesion.
- The difference between reflux and ulcers: In reflux, acid escapes into the esophagus; burning is felt mostly behind the breastbone. Pain in ulcers is usually in the upper middle part of the stomach (epigastric region).
- Ulcer pain in most people is of a burning-scratching type; in some people it increases with hunger, in others it becomes more pronounced after eating (this distinction may vary depending on the location of the ulcer).
Remember: Ulcers can sometimes progress silently. There is a risk of bleeding without symptoms, especially in the elderly or those who regularly take painkillers.
Differences Between Stomach Ulcers and Duodenal Ulcers
“stomach ulcer” and “duodenal ulcer**” (duodenal ulcer) are considered under the same umbrella as peptic ulcer, but there are some typical differences. Knowing these differences also clarifies questions such as “when does ulcer pain occur?”.
Fundamental differences (practical comparison)
- Timing of pain:
- Duodenal ulcer pain may increase in many people when they are hungry or at night; eating may provide temporary relief. For this reason, the question “is stomach pain at night an ulcer?” comes up frequently.
- Stomach ulcer pain may become more pronounced in some people after eating; decreased appetite may be seen.
- Weight change:
- Since pain may increase after a meal in stomach ulcers, some people may be prone to weight loss.
- Because pain in duodenal ulcer increases when hungry, some people may eat more often and gain weight (not always).
- Follow-up approach:
- In gastric ulcers, physicians may sometimes want to confirm healing with control endoscopy and biopsy if necessary.
- Risk of complications:
- Both types of ulcer can bleed. However, which patients are at higher risk depends on age, comorbidities, medication use (especially NSAIDs), smoking and H. pylori status.
This distinction is not a diagnostic substitute, but is helpful in interpreting symptoms. Especially if symptoms of stomach ulcers or symptoms of duodenal ulcers are suspicious, a physician evaluation is important for a correct diagnosis.
What are the Symptoms of Ulcer (Typical Complaints and Alarm Signs)
Ulcer symptoms may vary from person to person. While some people have mild burning, others may experience pain and nausea that affects daily life. Most common complaints:
- Upper abdominal pain/burning (epigastric pain): May be described as “scraping” or “burning”.
- **Indigestion, bloating, early satiety
- Nausea, sometimes vomiting
- Belching, heartburn (may be associated with reflux)
- Decreased appetite (especially in gastric ulcer)
- **In some people, the pain may radiate to the back; however, this finding alone does not prove ulcer.
Alarm signs: When to contact the emergency department?
The following symptoms may indicate serious complications such as ulcer bleeding or perforation. Urgent evaluation is needed without delay:
- Bloody vomiting or dark vomiting like coffee grounds
- Black stool (melena): “Is black stool a sign of ulcer?” is one of the most important answers to the question.
- Sudden onset of very severe abdominal pain (suspicion of perforation)
- Fainting, severe weakness, palpitations
- Unexplained weight loss, signs of anemia
- Difficulty swallowing, persistent vomiting
If you have these symptoms, do not expect them to “go away at home”.
What Causes Ulcers (H. pylori, Painkillers and Other Risks)
the answer to the question “**Does H. pylori cause ulcers?” Yes, it is one of the most common causes of peptic ulcer in the world. In addition, the second major cause is NSAID group painkillers.
1) Helicobacter pylori (H. pylori)
H. pylori is a bacterium that can settle in the stomach. By weakening the gastric mucosa and increasing the effect of acid, it may predispose to ulcer development.
- Transmission is usually associated with oral transmission, close contact and hygiene conditions.
- Diagnosis may involve a breath test, stool antigen test or biopsy during endoscopy.
- The aim of treatment is to destroy the bacteria; this is usually done with acid suppressant + antibiotic combinations (planned by the physician).
2) NSAIDs/Painkillers
“**Do painkillers cause ulcers?” Yes; the risk increases especially in long-term and uncontrolled use. NSAIDs can weaken the stomach’s protective mechanisms. The risk is higher when
- over 60 years old
- Previous history of ulcer/bleeding
- Use of blood thinners or cortisone
- Smoking, heavy alcohol use
In these people, the physician may plan preventive treatment (e.g. PPI) if necessary.
3) Smoking, alcohol and stress
- **Smoking can make ulcers harder to heal and increase the risk of recurrence.
- Alcohol may increase symptoms in some people.
- **Stress alone is not the main cause of ulcers, but it can be a trigger that increases the perception of pain and stomach complaints.
Ulcer Diagnosis and Ulcer Treatment: When is endoscopy needed and how many days does the treatment take?
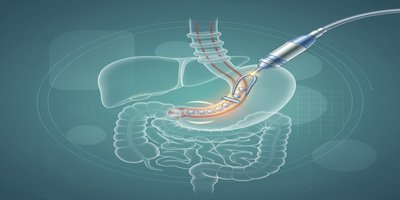
In suspected ulcer, the diagnosis is planned according to the duration of complaints, age, risk factors and alarm findings. The most accurate method is often endoscopy. Endoscopy allows direct visualization of the stomach and duodenum; a biopsy can be taken if necessary. (For details, see our article What is Endoscopy?)
When is endoscopy more recommended?
- If there are alarm findings (bleeding, weight loss, anemia, etc.)
- In new-onset complaints in advanced age
- In complaints that do not go away despite treatment
- When it is necessary to confirm healing in suspected gastric ulcer (physician’s decision)
How is ulcer treatment done?
Ulcer treatment depends on the cause of the ulcer:
- Acid suppressive therapy (such as PPI): Helps the wound heal by reducing stomach acid.
- Eradication treatment if H. pylori is positive: Antibiotic combinations + acid suppressant.
- In NSAID-induced ulcer: If possible, drug discontinuation/alternative plan, preventive treatment and risk management are performed (with physician guidance).
“How many days does ulcer treatment last?”
There is no single answer to this question; the location and size of the ulcer, the presence of H. pylori and the person’s risk factors affect the duration. Generally:
- Acid suppressive therapy is planned in weeks.
- H. pylori treatment is a specific cure, after which the physician will schedule a follow-up test if necessary.
Stopping medication early may increase the risk of ulcer recurrence, even if the symptoms improve. The most important part of treatment is compliance.
Nutrition and Lifestyle in Ulcers: Ulcer Diet, What Not to Eat, Myths-Facts
searches for “ulcer diet” and “what not to eat in ulcer” are very common. However, it would not be right to give a one-size-fits-all list for ulcers. Because triggers vary according to the person. Nevertheless, there are practical suggestions that work for most people:
General dietary recommendations
- Few and frequent meals may reduce pain in some people.
- Very hot/very cold food and drinks may increase sensitivity.
- Avoiding large meals late at night is helpful, especially if accompanied by reflux.
- A fatty, fried diet may increase the symptoms in some people.
Frequently asked questions
- **Does coffee increase ulcers? Coffee may increase stomach acid and burning in some people. Instead of a total ban, it is more realistic to reduce if your complaints are increasing.
- Bitter, spicy, acidic drinks: It does not have the same effect on everyone; however, if the burning increases, it makes sense to limit it.
- “Is milk good for ulcers? “ Milk may feel like a short-term relief; but in some people, it may increase acid secretion and trigger the complaint. It should not be seen as a permanent solution.
Lifestyle
- Smoking cessation can help heal ulcers and reduce recurrence.
- If you need to take painkillers (especially NSAIDs), discuss safe options with your doctor instead of using them “indiscriminately”.
- Regular sleep and stress management can reduce the perception of grievances.
Frequently Asked Questions (FAQ)
Is ulcer contagious?
Ulcers themselves are not contagious, but H. pylori, one of the major causes of ulcers, can be transmitted from person to person.
Can ulcers turn into cancer?
Not every ulcer is cancerous. However, especially in suspected gastric ulcer, the physician will perform endoscopy and biopsy if necessary. This approach is meant to exclude possible risks.
Will the ulcer recur?
Yes, the risk of recurrence may increase, especially if H. pylori treatment is not completed, smoking continues or NSAID use continues.
Does ulcer pain happen before or after eating?
This depends on the location of the ulcer: although it is more common for duodenal ulcer to become apparent when hungry/at night and for gastric ulcer to become apparent after a meal, it is not an absolute rule.
Conclusion: What is the Right Step in Suspected Ulcer?
as important as the answer to the question “**What is an ulcer?” is finding the cause of the ulcer and planning the right treatment. Stomach ulcers and duodenal ulcers can be treated most of the time; however, if there are alarming symptoms, immediate evaluation is essential. It is safest to consult a specialist if your symptoms persist for a long time, especially if ulcer symptoms have become regular or if you have a history of painkiller use.
Related content: What is H. pylori?, Symptoms of Stomach Bleeding, What is Endoscopy?
For medical informational purposes; gastroenterology/related physician evaluation is required for diagnosis and treatment.