What is ARMA (Anti Reflux Mucosal Ablation)? A Comprehensive Guide to Non-Surgical Reflux Treatment
Reflux (GERD) can reduce the quality of life in many people with complaints such as burning in the chest, bitter water in the mouth (regurgitation), a feeling of getting stuck in the throat, chronic cough and hoarseness. Most patients benefit from medications that suppress stomach acid (especially PPI group) as a first step; however, in some people, the complaints cannot be fully controlled, they come back quickly when the medication is stopped or the search for an alternative to long-term drug use begins. At this point, “non-surgical reflux treatment” and “endoscopic reflux treatment” options come to the fore more.
One of the methods that we have started to hear more frequently in recent years is the ARMA (Anti Reflux Mucosal Ablation) approach. the answers to questions such as “What is **ARMA?”, “How is the **ARMA procedure performed?”, “Who is suitable and who is not recommended?” are very important in terms of correct patient selection. In this article, we will address the curiosities about ARMA reflux treatment in a patient-oriented language, comparing its advantages-disadvantages and alternatives such as reflux surgery. (Note: This content is for informational purposes; consult your physician for diagnosis and treatment plan)
What is ARMA (The Logic of Anti Reflux Mucosal Ablation)
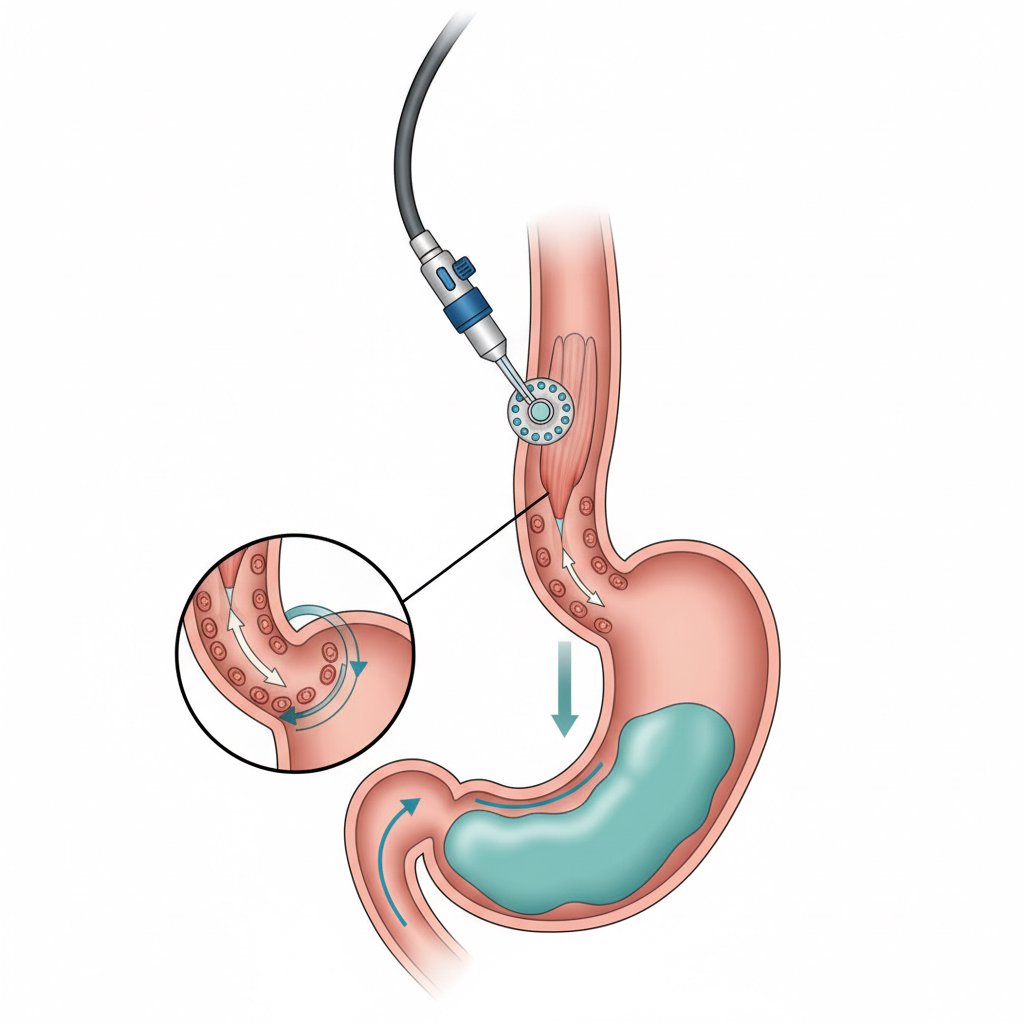
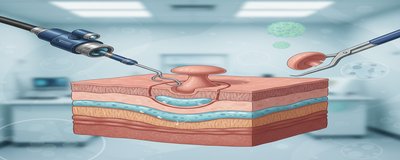
ARMA is an endoscopic reflux treatment approach that aims to reduce reflux at the esophagus-stomach junction (gastroesophageal junction) in gastroesophageal reflux disease (GERD). the word “ablation” is based on the idea that by performing a controlled superficial tissue treatment in the targeted area, the tissue shrinks and the barrier effect increases during healing. Simply put, the purpose of ARMA is to reduce the upward escape of stomach contents by creating a better closure/resistance in this transition zone where reflux often occurs.
Why is this important? The problem in reflux is often not only “excess acid”; structural factors such as weakening of the valve mechanism between the stomach and esophagus, increased relaxation, and in some patients hiatal hernia (stomach hernia) may also play a role. Therefore, reducing acid with medication alone may not completely resolve complaints with a strong mechanical component, such as regurgitation, in all patients.
At this point, ARMA is talked about as one of the non-surgical reflux treatment options that stand out with its “no incisions, no abdominal surgery” approach. However, there is a very critical point: ARMA is not suitable for everyone. One of the most important factors determining success is correct diagnosis and correct patient selection. Therefore, pre-procedural evaluation (endoscopy, 24 hour pH meter test if necessary, manometry, etc.) is often an integral part of the process.
How is the ARMA Procedure Performed (Step-by-Step Process, Sedation and First Days)
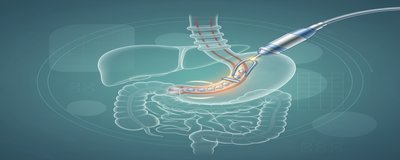
“ARMA procedure” is an endoscopic procedure; that is, it is planned by evaluating the stomach-esophagus junction area with an endoscope entered through the mouth. Although the details of the application may vary according to the center and the patient’s condition, the practical topics that patients are most curious about are generally as follows:
Pre-procedure evaluation
The likelihood of benefit from ARMA is closely related to the type and severity of reflux. Therefore, the physician will question your complaints and your response to the medication in detail. Frequently:
- Endoscopy is used to evaluate damage to the esophagus due to reflux, the presence of a hiatal hernia and accompanying problems.
- In some patients, objective measurement of reflux can be performed with 24 hour pH meter test.
- According to the complaints and clinical suspicion, esophageal manometry is requested and esophageal movements (motility) are evaluated.
At this stage, distinctions such as “is it reflux, functional indigestion or gastritis?” become clear. Because in non-reflux problems, the expected benefit from endoscopic reflux treatment methods such as ARMA may be limited.
Sedation/anesthesia and procedure duration
ARMA is usually performed under sedation (a state of sleep that increases patient comfort). The duration of the procedure may vary depending on the anatomy, accompanying findings and application technique. In many centers, same-day discharge can be planned; however, this decision is made by the physician based on the patient’s general condition and the need for post-procedure observation.
First 24-72 hours after the procedure: What is normal and when to consult a doctor?
Some complaints may occur for a short time after ARMA:
- Sensation of irritation in the throat (due to endoscopy)
- Temporary increase in chest burning/discomfort
- Tenderness in swallowing
- Mild nausea
However, you should seek medical attention without delay in the following cases: severe chest pain, bloody vomiting, black stools, high fever, increasing difficulty swallowing or shortness of breath.
In the post-procedure period, physicians usually give individualized recommendations about diet regimen, temporary use of acid-suppressing drugs and control plan. At this point, the answer to the question “Can I stop taking medication immediately after ARMA?” may vary from person to person; the goal is to reduce unnecessary medication use while controlling symptoms.
Related content: What is reflux? and What is endoscopy, how is it done?
Who is a Suitable Candidate for ARMA? Who is not recommended?
The most powerful area of ARMA is the reduction of reflux complaints in correctly selected patients. However, while answering the question “**What is ARMA”, it is also necessary to clarify the title “Who is it suitable for?”; because not all reflux patients experience reflux with the same mechanism.
Who does ARMA apply to? (General framework)
The following profiles may be candidates for ARMA according to the physician’s assessment:
- Those with reflux complaints that are partially relieved with medication but do not completely improve
- Especially those with marked mechanical escape sensations such as urgitation (bitter water in the mouth)
- Those with findings compatible with reflux in evaluations such as endoscopy/pH test
- people with suitable anatomy who want to evaluate non-surgical reflux treatment options before considering “reflux surgery”
Who may not be suitable?
ARMA is not the ideal choice for every patient. For example
- Endoscopic methods alone may be insufficient in patients with significant and severe hiatal hernia (gastric hernia).
- In patients with suspected severe esophageal motility disorder (evaluated by manometry), care should be taken in terms of swallowing problems after the procedure.
- The expected benefit may be lower in patients with complaints due to non-reflux causes (e.g. functional chest pain, hypersensitive esophagus).
Therefore, ARMA is not a “one-size-fits-all” solution; it is a individually tailored approach to endoscopic reflux treatment. The best results are seen in patients supported by accurate diagnostic tests and realistic management of expectations.
Internal link suggestion: What is the 24-hour pH meter test? and How does hiatal hernia affect reflux?
Advantages, Disadvantages of ARMA and Comparison with Reflux Surgery
The main reason for the popularization of ARMA is that it is seen as a less invasive option for patients seeking “non-surgical reflux treatment”. Nevertheless, it is important to know the limitations as well as the advantages when making a decision.
Advantages
- **Since it is an endoscopic reflux treatment, there is no incision in the abdomen.
- Recovery and return to daily life can be faster in most patients compared to surgery.
- In some patients, the need for medication may be reduced and significant relief of regurgitation complaints is targeted.
Disadvantages / limitations
- Not all reflux types are suitable for ARMA; it may not be sufficient alone, especially in patients with predominant anatomical problems.
- The results may vary from person to person; some patients may not completely stop needing medication.
- As with any medical procedure, there are risks (bleeding, pain, swallowing sensitivity, rarely more serious complications). These risks are assessed according to the experience of the center and the characteristics of the patient.
ARMA or reflux surgery?
“Reflux surgery” (e.g. fundoplication techniques) is usually an option that aims for more radical anatomical correction and may be considered especially in patients with significant hiatal hernia or advanced reflux. ARMA may be considered as a more minimally invasive alternative in the appropriate patient. The most accurate decision is made by the gastroenterology and/or general surgery specialist in conjunction with endoscopy findings, pH measurement and manometry results.
If you want to elaborate on this comparison, you can also take a look at this content: What is reflux surgery, who is it recommended for?
Nutrition and Lifestyle after ARMA: Steps to Strengthen the Outcome
In the post-ARMA period, dietary and lifestyle adjustments are important to support the benefits from the procedure. Your physician’s recommendations are always prioritized, but in general terms the following headings are commonly used:
Nutrition (general approach)
- In the first days, soft and easily consumed foods that do not tire the stomach can be preferred.
- Spicy, very fatty, very acidic foods and drinks and carbonated drinks may increase symptoms in some patients.
- Small and frequent meals, avoiding large portions at late hours help control reflux.
Lifestyle recommendations
- Finish eating 2-3 hours before bedtime
- Reducing excess weight (may reduce reflux by lowering intra-abdominal pressure)
- Quit smoking
- Raising the head of the bed (especially in those with nocturnal reflux)
ARMA alone should not be considered as a “magic bullet”. Just like medication or reflux surgery, the best results are usually achieved with the right patient selection + right follow-up + lifestyle support.
Frequently Asked Questions (FAQ)
Is ARMA permanent?
The effect of ARMA depends on the individual and the cause of the reflux. In some patients, long-term relief can be achieved; in others, symptoms may partially return over time and additional treatment may be required.
Can medication be stopped after ARMA?
In some patients, the need for medicines such as PPIs may decrease. However, it is not correct to say that “everyone remains drug-free”. Your doctor will plan the follow-up according to the symptoms and test results.
Is the ARMA procedure painful?
Since the procedure is performed under sedation, no pain sensation is expected during the procedure. Irritation in the throat, burning in the chest or swallowing sensitivity may occur for a short time afterwards.
Is ARMA possible with a hiatal hernia?
The degree of hernia is important. In small hernias, options can be discussed with the physician’s evaluation; in significant hernias, reflux surgery may be a more appropriate option.
Brief Note on Scientific Evidence and Safe Approach
Although ARMA is one of the methods attracting interest in the field of endoscopic reflux treatment, as with any new approach in medicine, the evidence may vary according to patient selection, application technique and follow-up period. Therefore
- To treat the results with personal assessment rather than seeing them as “definitive”,
- Questioning the experience of the team performing the procedure and the follow-up protocol,
- It is the healthiest approach to discuss alternatives (drug treatment, lifestyle, other endoscopic methods, reflux surgery) together.
Update note: This content is intended for patient information as of 2026; medical practices and guidelines may be updated over time.
For a case-specific evaluation of ARMA (Anti Reflux Mucosal Ablation), it would be the best step to consult a specialist with the duration of your complaints, your drug response, your endoscopy findings and, if necessary, your pH meter/manometry results.