What is Celiac Disease? Celiac Symptoms and Treatment (Gluten-Free Diet Guide)
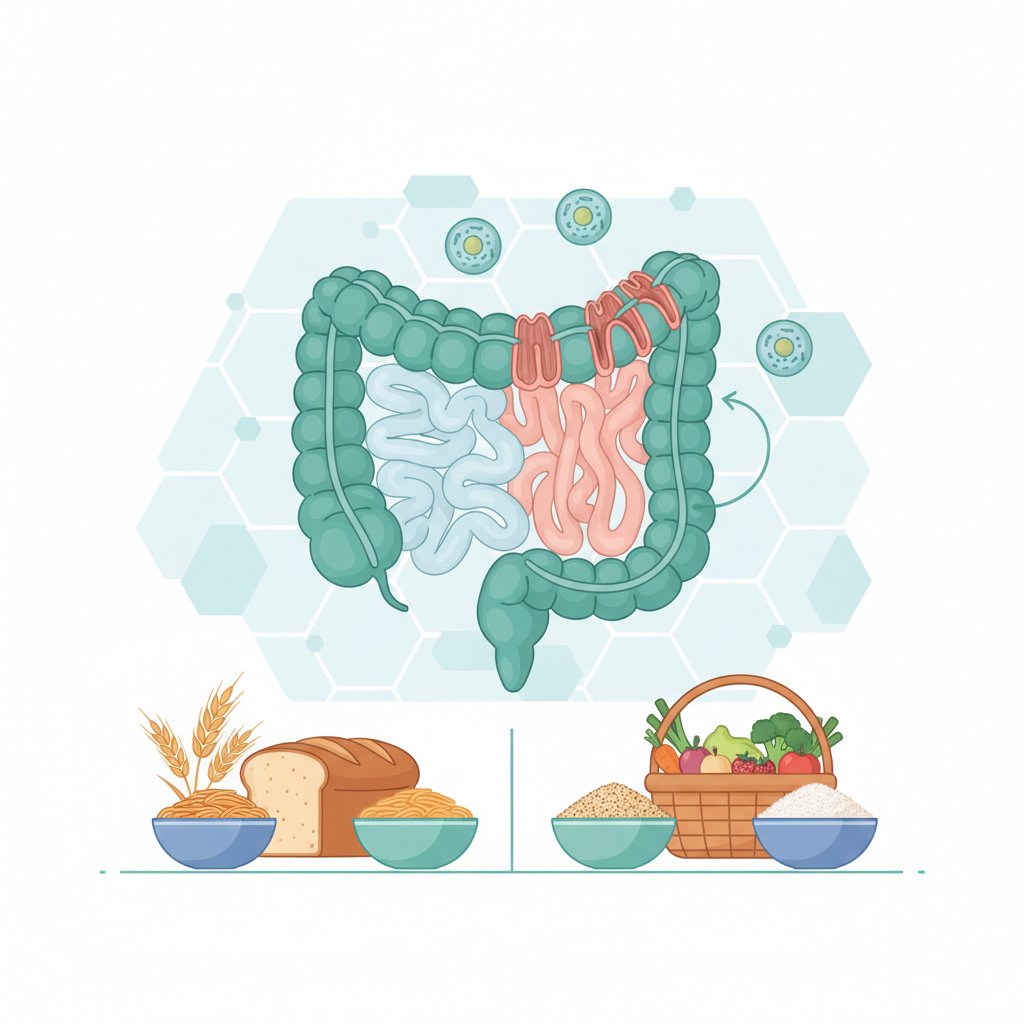
Celiac disease is an autoimmune disease triggered by gluten consumption. This means that the body’s immune system mistakenly attacks its own tissues when it encounters gluten. The small intestine is most affected: absorption of nutrients can be impaired because the absorption projections on the surface of the intestine, called “villi”, are damaged. As a result, not only digestive complaints such as abdominal pain and diarrhea, but also non-digestive symptoms such as iron deficiency anemia, growth retardation, weakness, skin rash may occur.
Many people confuse celiac disease with gluten intolerance. However, celiac disease is a serious condition that requires long-term follow-up and lifelong gluten-free diet and can be diagnosed with tests. In this article, you will find a comprehensive guide on “what is celiac disease”, “what are the symptoms of celiac disease”, “how to test for celiac disease” and “treatment of celiac disease (gluten-free diet)”. In particular, we aim to increase parents’ early awareness by giving special attention to celiac symptoms in children.
Note: This content is for informational purposes; consult a pediatric gastroenterology/internal medicine specialist for diagnosis and treatment plan.
What is Celiac Disease? Why is Gluten a Problem?
Celiac disease is characterized by damage to the small intestine caused by an autoimmune response to a protein called gluten. Gluten is found especially in wheat, barley and rye. Products such as bread, pasta, bulgur, bakery products made with these grains can trigger the immune system in people with celiac disease. As the villi are damaged in the small intestine, ** malabsorption develops, which can result in deficiencies of many nutrients such as iron, folate, B12, vitamin D, etc.
Celiac disease can occur at any age. In some people, symptoms begin in childhood, while in others they appear in adulthood. In so-called “silent celiac” or “atypical celiac”, classic digestive complaints may not be evident and the person may be followed for years with only anemia, decreased bone density or chronic fatigue.
Another important issue with gluten is the risk of cross-contamination. A gluten-free diet is not only about “not eating gluten-containing food”; it is also about preventing the gluten-free food from coming into contact with gluten. This is a critical detail that determines the quality of life in the celiac treatment process.
What are the Symptoms of Celiac Disease (in Children and Adults)?
Celiac symptoms may vary from person to person. In some people, digestive complaints are very prominent, while in others, non-digestive symptoms are more prominent. The following symptoms may suggest celiac disease:
Digestive symptoms (classic symptoms)
- Prolonged or recurrent diarrhea
- Constipation (especially in children, constipation may sometimes occur instead of diarrhea)
- abdominal pain, cramps
- abdominal distension and gas
- Weight loss, loss of appetite
- Nausea, vomiting (especially in young children)
Non-digestive symptoms (atypical/silent celiac)
- Iron deficiency and anemia (one of the most frequent clues)
- Chronic fatigue, weakness
- Aphthae in the mouth
- Bone and joint pain, vitamin D deficiency, osteopenia/osteoporosis
- Skin rash (dermatitis herpetiformis: itchy, blistering rash)
- Headache, difficulty concentrating, feeling of “brain fog”
- Reproductive health problems such as menstrual irregularities, infertility (in adults)
What are the symptoms of celiac disease in children?
One of the most frequently searched topics by parents is symptoms of celiac disease in children. In children, the picture can sometimes be more insidious. Signs to watch out for:
- Growth retardation, decrease in height-weight percentile
- Loss of appetite, picky eating, quick satiety
- Abdominal swelling (especially the appearance of a “drum-like abdomen”)
- Frequent illness, fatigue
- Iron deficiency anemia
- Decline in school performance, difficulty focusing, restlessness
- Deterioration/staining of tooth enamel
If your child has both digestive complaints and problems with growth and development, it is important to evaluate for celiac test before saying “gluten intolerance”. At this point, you can also take a look at our article nutrition and growth monitoring in children.
Celiac or Gluten Intolerance or Wheat Allergy (Differences)
although the term “gluten intolerance” is used a lot in everyday language, medically it can cover different conditions. The three most commonly confused tables are the following:
1) Celiac disease
- Mechanism: Autoimmune (the immune system damages the intestinal tissue)
- Diagnosis: Serologic blood tests + endoscopy/biopsy if necessary
- Risk: Complications such as nutritional deficiencies, growth retardation, bone health problems if left untreated
- Treatment: ** Lifelong gluten-free diet** + follow-up
2) Non-celiac gluten sensitivity (colloquially “gluten intolerance”)
- Mechanism: Not autoimmune; celiac tests are negative
- Diagnosis: Diagnosis of exclusion (assessed after exclusion of celiac and wheat allergy)
- Risk: Generally, intestinal damage as severe as celiac is not expected
- Treatment: Gluten reduction/removal according to the individual; dietitian support may be useful
3) Wheat allergy
- Mechanism: Allergic (may be IgE mediated)
- Symptoms: Rapid reactions such as itching, hives, shortness of breath, anaphylaxis may occur
- Diagnosis: Allergy tests (skin prick test, specific IgE, etc.)
- Treatment: Avoidance of wheat + allergist follow-up
In short: Celiac treatment and the need for follow-up is different from the generalized sensitivity to “gluten intolerance”. It is therefore safer to seek a correct diagnosis first, rather than cutting gluten on your own.
How is Celiac Diagnosed? Celiac Test and Points to Consider
the question “**How to test for celiac disease?” is especially important in children, because early diagnosis makes a big difference in growth and development. The diagnosis usually proceeds in the following steps:
1) Blood tests (serology)
The most commonly used tests are:
- tTG-IgA (tissue transglutaminase antibody)
- Total IgA (tests may be misleading if IgA deficiency is present)
- EMA-IgA (endomysium antibody) if necessary
These tests are the first step in the suspicion of celiac disease and require physician evaluation for correct interpretation.
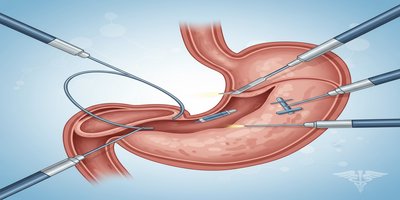
2) Endoscopy and biopsy (when necessary)
In some cases, especially if the clinical picture is inconsistent with blood tests or if the diagnosis needs to be confirmed, a biopsy of the small intestine may be taken by endoscopy. In some guidelines in children, a biopsy-free diagnostic approach may be considered under certain conditions; however, this decision must be made by a specialist.
3) Genetic testing (HLA DQ2/DQ8)
Genetic testing does not mean “if you have it, you definitely have celiac disease”, but if you don’t have it, the chance of having celiac disease is very low. It provides supporting information, especially in ambiguous situations.
Very important warning: Don’t cut gluten before the test
the answer to the question “Do I need to stop gluten to be tested for celiac disease?” is often no. Stopping gluten early can make blood tests and biopsy findings negative, which can delay the diagnosis. If you have symptoms, it is advisable to consult a specialist without stopping gluten until a test plan is in place.
For accompanying conditions such as iron deficiency in this process, our article iron deficiency symptoms can also be guiding.
Celiac Treatment: Gluten-Free Diet, Tracking and Daily Living Tips
when it comes to “Celiac treatment”, the basic approach is lifelong gluten-free diet. There is currently no drug treatment that completely eliminates celiac disease, but with the right diet and regular follow-up, the gut can heal and symptoms can be greatly reduced.
The basis of a gluten-free diet
Main sources of gluten:
- Wheat (flour, semolina, bulgur, pasta, most breads)
- Barley, rye
- Products that may be contaminated with gluten (some sauces, processed foods)
Naturally gluten-free foods:
- Meat, fish, eggs (if not breaded/coated)
- Dairy products (if unadulterated)
- Legumes, vegetables and fruits
- Rice, corn, buckwheat, quinoa
- Nuts (unless floured/coated)
Cross-contamination (gluten contamination) management
In celiac disease, even small amounts can cause problems for some people. Practical measures at home:
- Separate cutting board, separate toaster/toaster
- Not preparing at the same counter with flour products
- Not dipping bread in common spreads (jam, butter)
“Can oats be eaten in celiac disease?”
Oats themselves do not contain gluten, but may be contaminated with wheat during production/transportation. Therefore, only “certified gluten-free oats “ may be suitable for some people. Nevertheless, it is safer to proceed with the recommendation of a physician/dietician as personal tolerance may vary.
Shortcomings and follow-up
The following deficiencies are common in celiac disease due to malabsorption:
- Iron, folate, B12
- Vitamin D, calcium
- Zinc, magnesium
Therefore, blood values and growth-development (in children) should be monitored after diagnosis. Especially in children, it is important to plan gluten-free options for school/nursery nutrition and social environments. If you want, you can get practical ideas from our healthy nutrition recommendations at school age content.
When to consult a doctor (especially for children)
It is important to consult a doctor for evaluation for celiac disease if you have any of the following conditions
- Prolonged diarrhea/constipation, abdominal pain, abdominal distension
- Unexplained iron deficiency anemia
- growth retardation, failure to gain weight, loss of appetite in children
- Persistent fatigue, bone pain, recurrent canker sores
- Family history of celiac disease (increased risk)
Early diagnosis can be decisive for height growth, bone health, energy level and general development in children. If there is a suspicion of celiac disease, it is a better step to plan a celiac test first, instead of starting a diet on your own by saying “gluten intolerance may be present”.
Frequently Asked Questions (FAQ)
Will celiac go away?
Celiac is a chronic condition; it is not expected to “go away completely”. However, a gluten-free diet can control symptoms and heal intestinal damage.
Does a gluten-free diet make you lose weight?
The goal of a gluten-free diet is not to lose weight. Some packaged gluten-free products may even contain high calories. Dietitian support is recommended if there is a weight target.
Does celiac cause weight gain?
Weight loss may occur in untreated celiac disease due to malabsorption, but not always. Some people may gain weight as the bowel heals after diagnosis.
How many days do celiac symptoms appear?
Symptoms vary from person to person. Some people experience symptoms soon after ingesting gluten, while others may experience damage and symptoms over a longer period of time.
What should people with celiac disease not eat?
Wheat, barley, rye and products containing them should not be consumed. Label reading is also very important for processed foods where there is a risk of cross-contamination.
Celiac disease can be managed with proper diagnosis, regular follow-up and a well-planned gluten-free diet. If you think you or your child may have celiac symptoms, it is safest to consult a specialist without delaying the testing process.