What is EMR (Endoscopic Mucosal Resection)? How to do it? Risks, Preparedness and Recovery Guide
EMR (Endoscopic Mucosal Resection) is a less invasive treatment method compared to surgery that allows the removal of some lesions in the mucosal layer of the digestive tract (such as esophagus, stomach, colon) by endoscopy. many people researching “**What is EMR?” usually want to understand the options offered for polyps or superficial lesions detected during colonoscopy or gastroscopy. The main purpose of EMR is to both diagnose (pathology examination) and treat superficial lesions that may be at risk of cancer or caught at an early stage by completely removing them.
In this article, we will discuss the endoscopic mucosal resection method in a patient-friendly language: *how is the EMR procedure performed, to whom is it recommended, whether it is the same as endoscopic polyp removal, pre-procedure preparation, post-procedure recovery-nutrition, possible risks and factors affecting the price of EMR prices… We will also briefly mention ESD, which is often confused with EMR. (Note: This content is for informational purposes; you should consult your gastroenterology physician for personal medical decisions)
What is EMR? (Purpose and Basic Logic of Endoscopic Mucosal Resection)
Endoscopic mucosal resection (EMR) is the removal of lesions originating from the mucosa, the innermost layer of the digestive tract wall, using special devices advanced through the tip of an endoscope. One of the most common applications of EMR in colonoscopy: A more controlled removal is targeted compared to standard polypectomy, especially for broad-based (sessile) or larger polyps.
EMR has two important contributions:
- Therapeutic effect: The risk can be reduced by removing the polyp/lesion with cancerous potential.
- Diagnostic accuracy: The removed tissue is sent to pathology. questions such as “Is there dysplasia?”, “Are the borders clear?” become clear with the pathology report. Therefore, “endoscopic resection” is not only “polyp removal” but also a critical step that determines the future follow-up plan.
EMR is usually performed under sedation and most patients can be discharged the same day. However, factors such as the location, size, and number of lesions, the patient’s comorbidities, and the need for additional intervention during the procedure (e.g., bleeding control, clip application) may alter the process.
If you want to have a broader look at related topics, you can also check our pages: What is a colonoscopy? and [What is a polyp, why is it important?](/polyp-what is it)
In Which Situations Is EMR Performed (Indications) Who May Not Undergo EMR?
the answer to the question “Who can undergo EMR procedure?” depends on the characteristics of the lesion. In general, EMR is preferred in lesions that can be reached by endoscopy and are thought to be mostly superficial (limited to the mucosa).
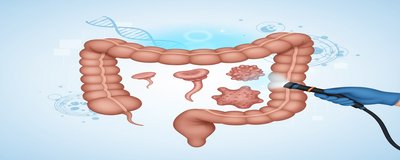
Colon polyps and broad-based lesions
- Colon polyp EMR applications are particularly relevant when it comes to the removal of large-based polyps.
- EMR technique may be more appropriate in lesions that are difficult to remove with standard “snare polypectomy”, have a larger area or are flat.
- The aim is to remove the lesion in the safest way possible and manage risks such as post-procedural bleeding.
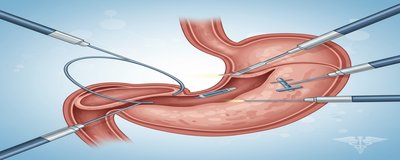
Gastric and esophageal lesions
- **EMR in the stomach or EMR in the esophagus may be performed in some superficial lesions (e.g. certain areas of dysplasia) if deemed appropriate by the physician.
- In these regions, the depth and boundaries of the lesion are very important; therefore, in some cases, different methods such as ESD instead of EMR may be considered.
Who is it not applicable to?
The final decision is based on the physician’s assessment, but in general:
- If the lesion is suspected to have spread to deeper layers,
- If the risk of bleeding is very high and cannot be regulated (e.g. certain blood thinners),
- If the general condition of the patient is not suitable for sedation/anesthesia,
- If safe endoscopic removal of the lesion is not possible, Different treatments can be planned instead of EMR.
A frequently asked question at this point: “Is endoscopic polyp removal the same as EMR? “ Not all polyp removal procedures are EMR. While some small stalked polyps can be removed by simple polypectomy, EMR is more commonly applied to selected lesions that require specific technical steps (such as submucosal fluid administration).
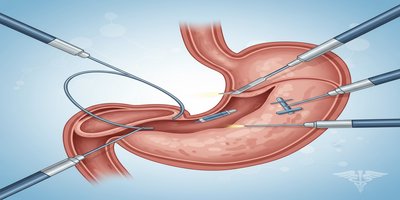
How to do EMR (Step-by-Step EMR Process)
the most understandable answer to the question “**How to do an EMR?” is to describe the process step by step. Although the application details may vary according to the center and lesion, the typical flow is as follows:
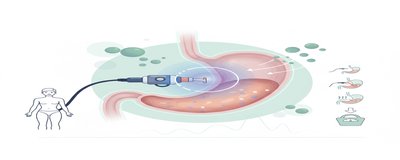
1) Sedation / anesthesia
Most of the time EMR is performed with sedation; the patient feels no or very minimal pain during the procedure. In some cases, deeper sedation with an anesthesia team may be preferred. It is generally recommended not to drive the same day after the procedure and to be accompanied.
2) Lesion assessment and planning
The borders, shape and removability of the lesion are evaluated with the endoscope. The physician decides whether to remove the lesion “in one piece” or “piece by piece”. (Some large lesions may require piece by piece removal; this may affect the follow-up plan.)
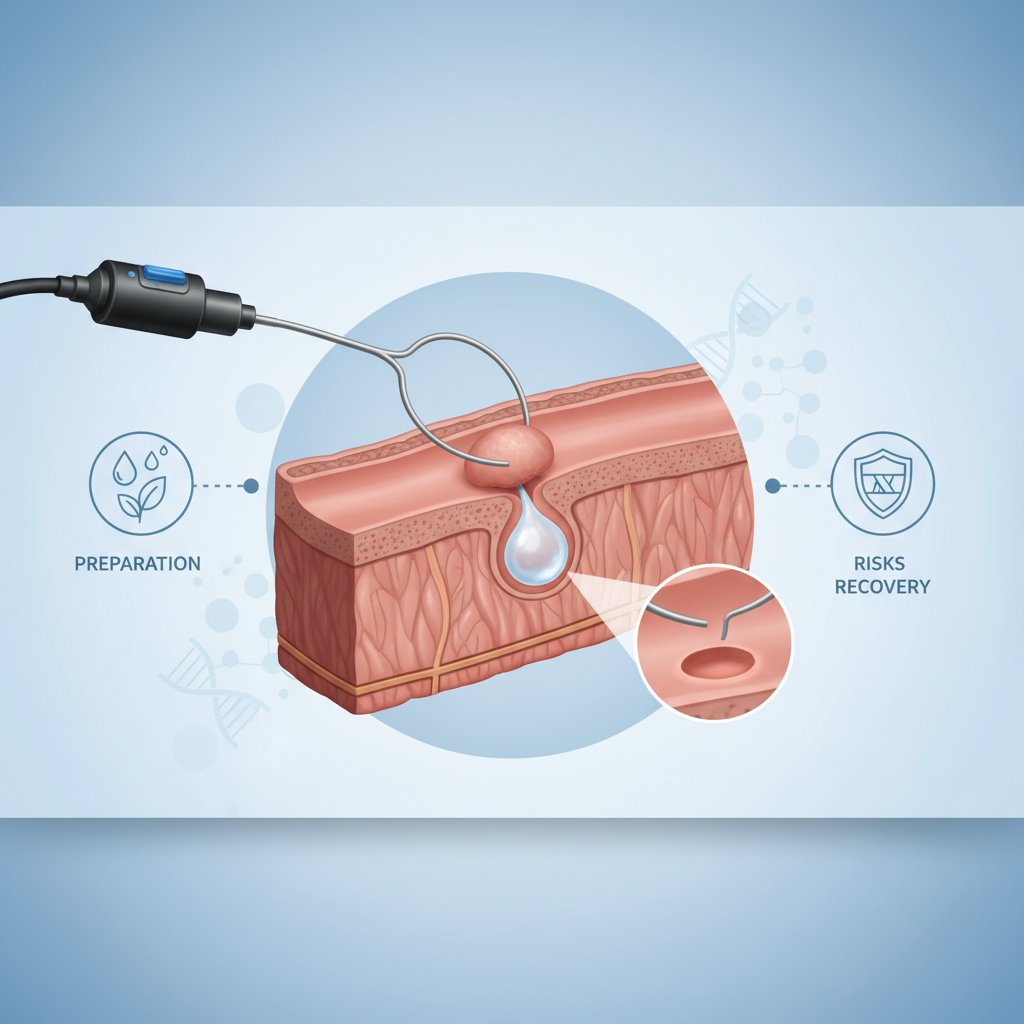
3) Submucosal injection (fluid administration under the mucosa)
One of the hallmark steps of EMR is submucosal injection. The area is “lifted” by introducing a special fluid under the lesion; this can facilitate removal and help reduce the risk of damage to deeper layers.
4) Resection (removal with snare)
The lesion is then captured with a ring-shaped device called a “snare” and cut out in a controlled manner. This stage can be thought of as a more advanced, technical version of “endoscopic polyp removal”.
5) Bleeding control and protective applications
If bleeding occurs in the procedure area, it can be controlled by endoscopic methods. When necessary
- Coagulation (incineration) methods
- Clip application
- Additional techniques to reduce bleeding can be used.
6) Referral to pathology
The removed tissue is always sent to pathology. the EMR pathology result determines the next step: Questions such as whether additional treatment is needed, how often follow-up should be, and whether the borders are clear are answered here.
EMR procedure duration varies according to the size/location of the lesion and additional interventions. For this reason, clear times such as “it takes x minutes” seen on the internet can be misleading.
Pre-EMR Preparation: Medications, Fasting, Bowel Cleansing (Checklist)
The safety of EMR is closely related to pre-procedure preparation. The following headings summarize the most frequently asked “Pre-EMR preparation” topics by patients:
Starvation period
- Your physician/center will tell you how many hours you should fast before the procedure. This time may vary depending on the type of sedation and the time of the procedure.
Bowel cleansing for the colon
- If EMR is planned in colonoscopy, bowel cleansing is critical. Inadequate cleaning can both make the lesion difficult to see and prolong the procedure time.
Blood thinners and other medicines
- Blood thinners such as aspirin, clopidogrel, warfarin or DOAC group drugs (some anticoagulants) should be discussed with the physician before the procedure.
- the answer to the question “Should I cut myself?” is usually no; the decision to cut/interrupt is planned with individualized risks.
- Diabetes medication/insulin use can also affect fasting and the day of the procedure.
Accompaniment and daily plan
- It is recommended not to drive the same day after sedation, not to make important decisions and to rest if possible.
For more detailed preparation steps: Pre-endoscopy preparation guide
Post EMR Process: Notes on Nutrition, Recovery, Follow-up and EMR Prices
Recovery and nutrition after EMR
“**Nutrition after EMR” may vary depending on the person and the area where the procedure is performed. In general
- Oral intake may be restricted in the first hours until the sedation effect wears off.
- If your doctor deems it appropriate, softer foods that do not tire the stomach/intestines may be recommended at the beginning.
- Some patients may experience bloating, gas and mild cramping.
**This depends on the extent of the procedure. In simple cases, it may be possible to return to daily activities the next day; in larger resections, your physician may ask you to take it easy for a few days.
Possible risks and “when to seek emergency care?”
EMR is generally considered safe, but like any medical procedure, there are risks. The most discussed ones are:
- Risk of bleeding: It may occur during or after the procedure.
- Perforation risk: It is rare but an important complication.
- Post-polypectomy syndrome-like abdominal pain/fever (not in all patients).
Contact your healthcare provider without delay in the following cases
- Severe/increased abdominal pain
- Fainting, marked weakness
- Intense rectal bleeding or bleeding with clots
- High fever, chills
- Black tarry stools (especially after upper GI procedures)
Pathology result and follow-up plan
the EMR pathology result usually determines the timing of the next follow-up. In some patients, a follow-up endoscopy/colonoscopy may be scheduled earlier. Your physician will create a personalized follow-up scheme based on the type of lesion, completeness of the extraction and pathology findings.
EMR or ESD? Short comparison
Another common question asked by patients is “EMR or ESD?”. In general terms:
- EMR is a widely used modality for selected superficial lesions.
- ESD may be a more technically advanced method that can target one-piece removal in some lesions.
Which method is appropriate is determined by factors such as the size and location of the lesion, suspicion of depth and center experience. (For detailed comparison: What is ESD, EMR-ESD difference)
EMR prices: What does it depend on?
you may want to see a clear figure for “EMR prices” on the internet, but the right approach is to know the factors affecting the price and wait for clarification after the examination/pre-assessment. The main factors that can affect the price of EMR are:
- Number, size and location of the lesion (colon, stomach, etc.)
- Sedation/anesthesia requirement of the procedure
- Additional materials used (e.g. clips)
- Hospital/center infrastructure, hospitalization requirement
- Pathology and additional examinations
- SSI/private insurance coverage and policy details
The best information on this subject is provided by the physician’s assessment and information from your center. For the pre-appointment process: Gastroenterology appointment and evaluation
Frequently Asked Questions (FAQ)
Is EMR painful?
Most patients experience no or minimal pain during the procedure due to sedation. Mild cramping/swelling may occur after the procedure.
Is bleeding after EMR normal?
Mild spotting bleeding may occur in some cases; however, intense, clotted or increased bleeding is not considered normal and requires urgent evaluation.
When is a follow-up colonoscopy performed after EMR?
It depends on the characteristics of the lesion and the pathology result. Your physician determines your personal follow-up interval.
Does EMR need to be repeated?
In some large lesions there may be a risk of recurrence/residue (tissue left behind); therefore follow-up endoscopy is important. Additional endoscopic treatments can be planned if necessary.
This guide aims to provide a comprehensive answer to the questions “What is EMR?” and “How is EMR performed?”. For the most appropriate approach in your case, it is best to contact your gastroenterologist and ask for a personalized plan based on the characteristics of the lesion.