What is ERCP? How is ERCP Procedure Performed? Biliary Tract Diseases and Treatment
Problems with the bile ducts and pancreatic duct can lead to complaints such as warmness, upper right abdominal pain, fever, chills, dark urine and light colored stools. Although these symptoms often seem like “simple indigestion”, there may be more serious underlying conditions such as biliary obstruction, choledochal calculi (stones in the bile duct), cholangitis (bile duct infection) or stenosis. At this point, ERCP (Endoscopic Retrograde Cholangiopancreatography) is an important interventional procedure that both helps to diagnose and is often used for treatment purposes.
In this article, we will address the most frequently asked questions such as “What is ERCP?”, “How is ERCP performed?”, “How is gallstone removal with ERCP?”, “When is biliary stent inserted?” in a patient-friendly language. You will also find clear and practical information about MRCP ERCP difference, pre-procedure preparation, post-procedure considerations and ERCP complications. (For more detailed reading, you can also check our Gastroenterology page and Endoscopy procedures guide
What is ERCP (Endoscopic Retrograde Cholangiopancreatography)?
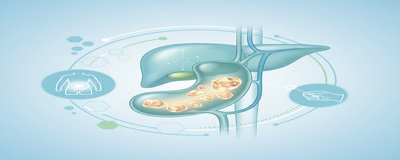
ERCP is a procedure that uses a flexible tube with a camera at the end (endoscope) and X-rays (fluoroscopy) to access the biliary ducts and pancreatic duct. ERCP, whose medical name is endoscopic retrograde cholangiopancreatography, is mostly performed for treatment purposes today. In other words, it is preferred not only for taking images but also for interventions such as opening the blockage, removing the stone, widening the stenosis or inserting a stent.
The main objectives of ERCP are:
- To reveal the cause of biliary obstruction and, if possible, to eliminate it in the same session
- **To reduce jaundice and pain by removing choledochal stones, if any
- Taking a sample (brushing/biopsy) in suspected biliary stricture (benign or malignant)
- to relieve the duct and help the healing of the leakage area in cases such as Bile leakage
- Maintaining the flow by placing a biliary stent when necessary
ERCP is a highly effective method when performed in the right patient with the right indication. However, since it is an interventional procedure, it is not applied “routinely” to every patient; the need is usually clarified beforehand with imaging such as ultrasound, CT or especially MRCP.
In Which Conditions Is ERCP Performed? Relationship with Biliary Tract Diseases
The most common area of ERCP is biliary tract diseases. The bile duct is like a “pipe system” that carries bile from the liver to the intestines. When there is an obstruction in this system, such as a stone, stenosis or tumor, bile flow is impaired and symptoms occur.
Indications for ERCP in biliary tract diseases
- Choledochal stone (bile duct stone): Stones in the gallbladder can sometimes fall into the common bile duct. This can lead to jaundice, pancreatitis or cholangitis. Stone removal by ERCP is an effective treatment in most patients.
- Septal obstruction and jaundice: Findings such as jaundice (yellowing of the skin and whites of the eyes), dark urine, itching, light-colored stools suggest obstruction. The location and cause of the obstruction can be evaluated by ERCP and a stent can be applied if necessary.
- Cholangitis: The association of fever, chills, jaundice and abdominal pain requires urgent evaluation. In some cases of cholangitis, bile drainage with urgent ERCP may be life-saving.
- Biliary strictures: Previous surgeries, inflammatory diseases or tumors can cause stricture. With ERCP, a stent can be placed in the stenosis area and in some cases a sample can be taken.
- Bile leakage: Especially in bile leakage that may develop after gallbladder surgery, stenting with ERCP may support the healing of the leakage area.
Pancreas-related conditions
ERCP can also be used in selected cases for pancreatic duct problems (duct strictures, duct stones, etc.). However, EUS (Endoscopic Ultrasound) or MR-based methods are often preferred for diagnostic evaluation of the pancreas; ERCP is more treatment-oriented.
How to Perform ERCP Procedure (Step by Step Explanation)
the question “**How is ERCP done?” is naturally one of the most curious topics. Although the details of the procedure may vary depending on the center and the patient, the general flow is as follows:
1) Preparation before ERCP
- Fasting: You are usually asked to fast for 6-8 hours before the procedure (time including water may vary depending on the physician/center).
- Blood thinners: Be sure to inform if you are taking medications such as aspirin, clopidogrel, warfarin, new generation anticoagulants. Planning is important as some interventions (e.g. sphincterotomy) may increase the risk of bleeding.
- Diabetes medications/insulin: Dose adjustment may be required due to fasting.
- Allergy, pregnancy, previous anesthesia problems: Contrast material, drug allergies or suspicion of pregnancy must be shared.
2) Sedation / anesthesia
ERCP is usually performed under sedation or general anesthesia in some patients. The aim is to increase the comfort of the patient and to carry out the procedure in a safe and controlled manner. the answer to the question “Does ERCP hurt?” is important here: With appropriate sedation, most patients feel no or very minimal pain during the procedure.
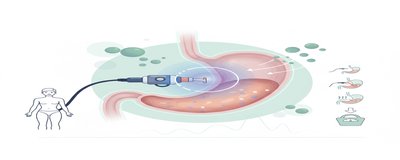
3) Technical stages of the process (simplified)
- The endoscope is advanced through the mouth, passes through the stomach and reaches the duodenum (duodenum).
- There is a region (papilla) where the bile and pancreatic duct opens.
- A thin catheter is inserted into the canal (cannulation).
- A contrast medium is administered and the ducts are visualized by fluoroscopy.
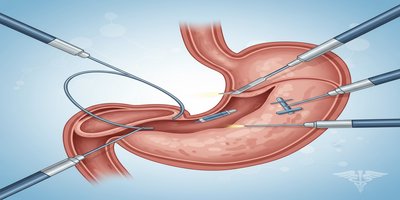
- Depending on the problem, intervention can be performed in the same session:
- Sphincterotomy/papillotomy: The canal mouth can be widened by cutting the papilla.
- Removing choledoch stones: Stones can be removed with a balloon or basket.
- Placement of a bile duct stent: A stent can be inserted to ensure flow.
- Sampling may be performed in case of suspected stenosis.
4) How long does ERCP take?
The duration of the procedure depends on the finding, the size of the stone, the location of the stenosis and the difficulty of cannulation. Simple procedures take a shorter time, while difficult cases may take longer. The team planning the procedure provides the most accurate information.
What is the Difference Between MRCP and ERCP?
Patients often ask “MRCP or ERCP?”. It is useful to make a short and clear distinction:
-
MRCP (Magnetic Resonance Cholangiopancreatography):
- It is non-invasive (no device is introduced into the body).
- It is used to visualize the bile and pancreatic ducts.
- It helps to diagnose, not treat.
-
ERCP:
- It is an interventional procedure (endoscopy + X-ray).
- It can diagnose but its main power is in treatment (stone removal, stenting, drainage).
- Therefore, the risk of complications is higher than with MRCP.
General approach: ERCP is planned if the suspicion of obstruction is strong on imaging and intervention is needed. In some patients, a “map” can be made with MRCP first and then targeted ERCP can be performed.
Post ERCP Process: Nutrition, Recovery and Cautions
The post-ERCP process varies according to the intervention performed (such as whether only imaging was performed, whether a stone was removed, whether a stent was inserted). Nevertheless, general recommendations can be summarized as follows:
First hours and same day
- You may be under observation for a while due to sedation.
- Mild throat irritation, flatulence or mild nausea may occur.
- regarding “nutrition after ERCP”, most centers recommend starting with clear liquids such as water and returning to normal as tolerated.
Things to watch out for at home
- It is recommended not to drive and not to make important decisions on that day (sedation effect).
- Mild fatigue may be normal, but severe abdominal pain, recurrent vomiting, increasing bloating are not considered normal.
- If a stent is implanted, the control plan (when the stent will be replaced/removed) should be determined by your physician.
When to contact the emergency department?
The following findings may be warning signs of ERCP complications and should be evaluated without delay:
- Severe or increasing abdominal pain (especially in the back)
- Fever, chills
- Constant vomiting, inability to feed by mouth
- Black stools, bloody vomiting or obvious signs of bleeding
- Increased jaundice, marked dark urine
Risks and Possible Complications of ERCP (A Realistic and Transparent View)
ERCP is usually planned by considering the benefit-risk balance. Nevertheless, since it is an interventional procedure, there are some risks. The most known complications:
- Post-ERCP pancreatitis: Pancreatitis may develop after the procedure; it is characterized by abdominal pain and enzyme elevation.
- Bleeding: It can be seen especially in patients undergoing sphincterotomy.
- Perforation (perforation): It is a rare but serious condition.
- Infection (cholangitis): May develop if drainage is insufficient or in some risky situations.
- Sedation/anesthesia-related risks: Conditions such as respiratory suppression require more careful monitoring, especially in patients with comorbidities.
Experienced team, appropriate patient selection, pre-procedural preparation and some preventive approaches (protocols varying according to the patient) are important to reduce the risks. Therefore, the decision for ERCP should be made individually, if possible together with the gastroenterology/endoscopy team.
Frequently Asked Questions (FAQ)
Does ERCP hurt?
Pain during the procedure is minimal as it is performed under sedation in most patients. There may be mild discomfort after the procedure; severe pain should be evaluated.
Is gallstone removal by ERCP a definitive solution?
**Choledochal stones are often successfully removed by ERCP. However, predisposition to stone formation may persist; underlying causes and gallbladder condition (surgical plan if stones are present) are important.
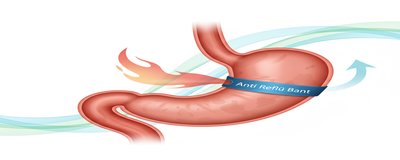
What is a bile duct stent and when is it inserted?
**A bile duct stent is a small tube that is inserted into the duct to maintain the flow of bile in case of stenosis or obstruction. There may be plastic or metal options; which is appropriate depends on the disease.
When can I return to work after ERCP?
Due to sedation, rest is usually recommended on the same day. Most people can return to daily life the next day; however, the intervention performed and the general condition are decisive.
When Should You Consult a Doctor?
If you have the following symptoms, it is important to be evaluated for biliary tract diseases without delay:
- Jaundice, itching, dark urine, light-colored stools
- Fever + chills + abdominal pain (urgent for cholangitis)
- Severe abdominal pain or recurrent vomiting
- If ERCP has been performed before and complaints are increasing
You can contact us from our Contact page for appointment and evaluation process or you can review the Gastroenterology section for relevant branch information.
Medical warning: This content is for informational purposes; it is not a substitute for diagnosis and treatment. The most accurate decision for procedures such as ERCP is made by your physician after examination and examinations.