What is ESD (Endoscopic Submucosal Dissection)? What are the Advantages?
While in the past some lesions of the digestive system (e.g. early stage tumors or large polyps in the stomach, esophagus or large intestine) were often removed surgically, today less invasive options have become possible thanks to endoscopic surgery methods. One of these methods is ESD (Endoscopic Submucosal Dissection). So what is ESD, how to make ESD transactions and what are the ESD advantages?
In this article, we will answer the most frequently asked questions of patients in a patient-friendly language: In which cases ESD is preferred, differences with EMR, pre-procedure preparation, possible risks, recovery process and nutrition after ESD. Remember: Health content is for general informational purposes; the best decision is made by the gastroenterologist who evaluates criteria such as the location/size of the lesion and suspicion of pathology.
What is ESD (Endoscopic Submucosal Dissection)
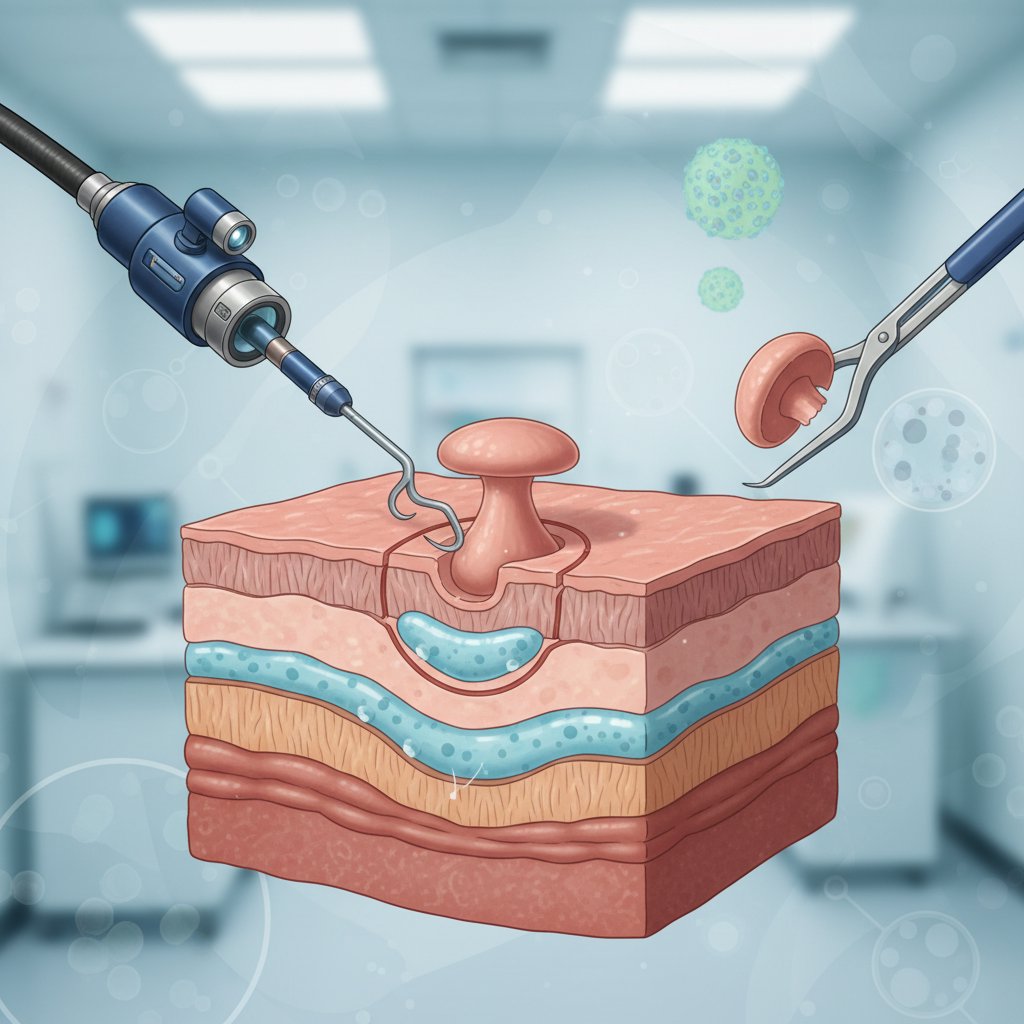
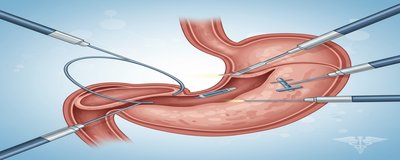
ESD (endoscopic submucosal dissection) is an advanced endoscopic treatment method that aims to remove the lesions located on the inner surface (mucosal layer) of the digestive tract, which are usually caught in the early stages, with the help of an endoscope. “Endoscopic” means that the procedure is performed with an endoscope inserted through the mouth or anus; “submucosal dissection” means that the lesion is removed by careful dissection of the underlying submucosa.
The most important aspect of ESD for patients is the following: When the lesion can be removed in one piece, pathology evaluation can be performed more accurately. This helps to report critical results such as “complete resection (R0 resection)” more clearly. Therefore, ESD stands out as an organ sparing approach in the appropriate patient.
ESD is not open/laparoscopic surgery in the classical sense, although it is referred to with the word “surgery”; it can be considered more as advanced endoscopic surgery. Nevertheless, it is a technically challenging procedure and requires an experienced team, appropriate equipment and correct patient selection.
Related reading: For general information about endoscopic procedures, you can check our pages [What is endoscopy?]( /endoscopy-what is it ) and for colonoscopy screening Colonoscopy guide.
In Which Situations Is ESD Applied (To Whom Is It Applied, To Whom Is It Not?)
the answer to the question “**Who should undergo ESD?” is closely related to the location, size, depth and carcinogenesis risk of the lesion. In general, ESD is preferred for superficial (early stage) and limited lesions, especially when one-piece removal is important. Application areas vary according to the physician’s assessment, but may include
Frequently assessed areas
- Gastric lesions: Suspicion of early stage gastric cancer, dysplasia, large superficial lesions
- Esophagus: Dysplasia and early stage lesions (e.g. on the background of Barrett’s)
- Colon and rectum: Large/difficult to localize polyps or early stage superficial lesions
Who may not undergo ESD? (Contraindications)
Not all patients are suitable for ESD. For example:
- Suspicion of deep invasion of the lesion (possibility of more advanced stage)
- Uncontrolled conditions that increase the risk of bleeding
- Some anatomical/clinical conditions that make the procedure difficult
- The general condition of the patient is not suitable for sedation/anesthesia
At this point, the aim is not “ESD for everyone”, but the right method for the right patient approach. Sometimes EMR (endoscopic mucosal resection) may be sufficient; sometimes surgical options may become safer and more effective.
Related reading: You can also review our article Polyp removal methods (EMR) to understand the options in polyp treatments.
How to Perform ESD (Step-by-Step Process, Duration and Preparation)
the ESD procedure is usually performed in the endoscopy unit under sedation or anesthesia, depending on the patient’s condition. the question “**Does *ESD hurt?” becomes important here: The patient usually does not feel pain during the procedure; however, complaints such as mild pain, burning, swelling in the post-procedure period may vary from person to person.
1) Preparation before ESD
Preparation may differ according to the region where the procedure will be performed:
- Fasting time: For stomach/esophageal procedures, a certain number of hours of fasting is required.
- Bowel preparation for colon: Colonoscopy-like cleaning may be required.
- Medications: Planning is very important especially in patients on blood thinners. Discontinuation/resumption of medications must be done with the physician’s advice.
- Necessary blood tests and anesthetic evaluation may be ordered.
2) Basic steps of the process (simplified explanation)
- The borders of the lesion are assessed with an endoscope and can be marked.
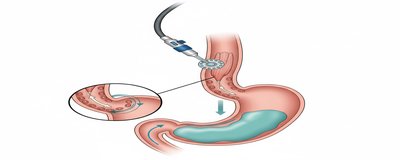
- The lesion is “lifted” by introducing fluid under the mucosa (to create a safer dissection plan).
- Incisions are made around the lesion.
- with submucosal dissection, the lesion is carefully separated from the underlying tissues.
- The removed tissue is sent to pathology (for diagnosis and “full extraction” evaluation).
3) How long does ESD last?
there is no single answer to the question “**How long does ESD last?”. The duration varies according to factors such as the size of the lesion, its location, vascular structure, whether it has been previously treated or not. Some procedures may take less time, while technically difficult cases may take longer. Your doctor will give you a more precise range for your particular case.
4) What does pathology and “R0 resection” mean?
One of the goals of ESD is to remove the lesion in one piece and send it to pathology with “clean margins”. Pathology report
- Type of lesion
- Whether the boundaries are clear (such as R0)
- Depth and risk criteria and other information. This information is critical in determining whether additional treatment is needed.
What are the Advantages of ESD (Why is it Preferred?)
the advantages of ESD may be quite evident in the appropriate patient. However, it is important to remember that every advantage depends on the right patient selection and experienced team.
1) Probability of en-bloc inference
One of the greatest strengths of ESD is the goal of removing the lesion in one piece. In this way:
- The pathologist can evaluate the lesion more clearly,
- The cleanliness of borders can be reported more accurately,
- In some cases, the risk of recurrence may be reduced (depending on case characteristics).
2) Organ-preserving approach
Compared to surgery, ESD can help preserve the organ in appropriate cases. For example, in regions such as the stomach or rectum, correctly selected early-stage lesions can be treated with less tissue loss.
3) Less invasive endoscopic surgery
Because ESD can be performed without abdominal opening or large incisions:
- The healing process can be more comfortable,
- The hospital stay may be shorter in some patients,
- Return to daily life may be faster (depending on the individual).
4) Managing treatment and diagnosis together
In some lesions, ESD can both provide treatment and provide important information for “definitive diagnosis and staging” by pathology. This guides the physician in planning the next steps.
ESD or EMR? Differences + Risks and Post ESD Process
One of the most frequently searched topics by patients is “ESD EMR difference “. In short:
- EMR (endoscopic mucosal resection) is generally a method for more superficial and/or smaller lesions, where piecemeal removal is acceptable in some cases.
- ESD is more prominent in larger lesions or lesions with more critical margins, where single piece extraction is important; it is technically more difficult.
ESD and EMR comparison table (general framework)
| Feature | EMR | ESD |
|---|---|---|
| Objective | To remove the lesion endoscopically | To remove the lesion one piece if possible |
| Technical difficulty | Relatively easier | Requires more advanced expertise |
| Single piece extraction in large lesions | More limited | More likely |
| Pathology evaluation | May be more difficult if it is fragmented | May be clearer if it is one piece |
| Duration | Shorter in most cases | May be longer depending on case difficulty |
ESD risks and possible complications
Like any medical procedure, ESD has risks. The most frequently discussed are:
- Bleeding: May occur during or after the procedure.
- Perforation (perforation): It may develop rarely; sometimes it can be closed by endoscopic methods, sometimes additional intervention may be required.
- Stenosis (especially after esophageal ESD): May present with dysphagia.
**If there are symptoms such as severe abdominal pain, fainting, intense bleeding, high fever, black stools, chest pain, you should immediately consult a health institution.
Post-ESD: recovery, follow-up and nutrition
- Hospital stay: It may vary according to the location of the procedure and risk status.
- Nutrition after ESD: In esophageal/gastric procedures, a liquid-soft food plan may be considered for a while; recommendations may be different in colon procedures. The most accurate list is the written instructions given by the team performing the procedure.
- Follow-up and pathology result: Depending on the pathology result, additional treatment, follow-up endoscopy or only follow-up plan can be made.
- Return to work: Depends on the individual recovery rate, the extent of the procedure and the doctor’s recommendation.
Frequently Asked Questions (FAQ)
Is ESD surgery or endoscopy?
ESD is an endoscopic procedure that does not require an incision like conventional surgery, but is also referred to as endoscopic surgery because it is “advanced”.
Can bleeding occur after ESD?
It can happen. Mild bleeding can be seen in some cases; if there are symptoms such as heavy bleeding or weakness/fainting, urgent evaluation is required.
When can I eat after ESD?
It depends on the area where the procedure was performed. In some patients, fluid can be started on the same day, while in some cases it is more cautious. The plan recommended by your doctor should be followed.
Does ESD completely cure cancer?
ESD can be curative in appropriately selected early stage lesions, but this depends on the pathology report and risk criteria. The “definitive” answer is therefore individualized.
Conclusion Making an Informed Decision about ESD
Endoscopic submucosal dissection (ESD) is a powerful option for the treatment of early stage gastrointestinal lesions in appropriate patients. summary of What is ESD: It is an advanced method of endoscopic surgery that aims to provide both treatment and sound pathology evaluation by removing the lesion with an endoscope, often in one piece. The best results are achieved with the right indication, experienced team, good preparation and regular follow-up.
It is important to consult your gastroenterologist for personalized information on pre-appointment preparation, procedure plan and nutrition after ESD. You can also review the basic process through our [What is endoscopy?]( /endoscopy-what is it ) and Colonoscopy content if you want to go prepared.