What is Fundal Ablation? Endoscopic Obesity Treatment Method (Who is Suitable, How is it Performed, Risks)
When it comes to obesity treatment, interest in “non-surgical” or “less invasive” options has been increasing rapidly in recent years. One of the prominent methods at this point is fundal ablation. So what is fundal ablation, how is it applied and for whom is it really a suitable endoscopic obesity treatment option?
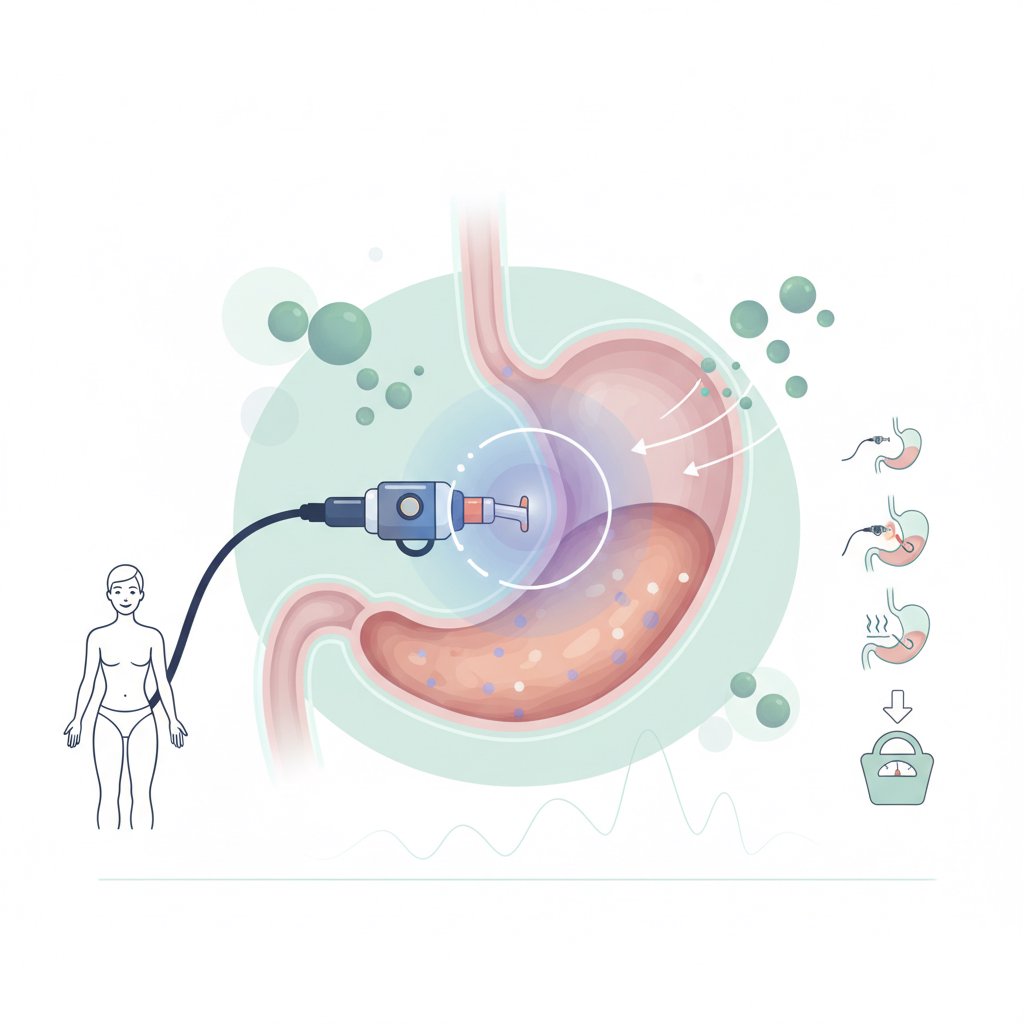
Fundal ablation (also referred to as gastric fundus ablation in some sources) is a procedure performed with the help of endoscopy to the fundus region located in the upper part of the stomach. The aim is to support the endoscopic weight loss process by targeting mechanisms that may affect appetite, satiety and eating behavior. Of course, this is not a “miracle alone” solution: The best results are achieved with physician follow-up, a nutrition plan and lifestyle changes.
In this article, we will discuss the rationale of fundal ablation, procedure steps, suitable candidates, possible risks and differences with other endoscopic weight loss methods in a patient-friendly language. (For a broader framework, you can also take a look at our obesity treatment guide)
What is Fundal Ablation? Why is the Stomach Fundus Important?
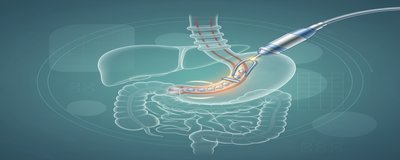
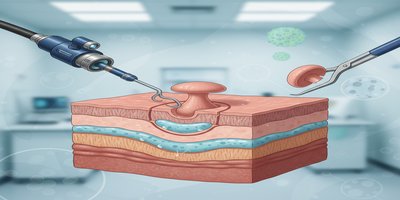
Fundal ablation is based on a controlled application to a specific area in the upper part of the stomach called “fundus” by endoscopic method. the term “endoscopic” means that the procedure is performed through an endoscope inserted through the mouth without an incision in the abdomen. Therefore, fundal ablation should not be confused with classical bariatric surgeries (e.g. sleeve gastrectomy).
What is the gastric fundus?
The stomach is anatomically divided into several parts. the Fundus is the dome-shaped region in the upper-left part of the stomach. This is an area associated with gastric capacity, distension sensation and some hormonal/appetite-regulating processes. Therefore, the concept of “gastric fundus ablation” was born from the idea of targeting that could support appetite and satiety management.
What is fundal ablation not?
- it is not a gastric balloon (no temporary balloon is inserted into the stomach).
- It is not endoscopic stomach reduction / endoscopic sleeve gastroplasty (ESG) (the stomach is not given a tube shape with sutures).
- it is not Bariatric surgery (stomach tissue is not removed, there is no incision).
It is important to know this distinction because it is very common for patients to confuse methods in their search for “endoscopic weight loss”. If you want, you can go to our endoscopic obesity treatment methods page to read other options comparatively.
How Fundal Ablation Works (Mechanism, Appetite and Satiety Relationship)
The goal of fundal ablation is to support the processes of appetite control and feeling of fullness through the application in the fundus region of the stomach. The most curious issue here is the relationship with ghrelin, commonly known as the “appetite hormone”. It is known that the hormone ghrelin originates from the stomach and plays a role in appetite signals; however, hormone levels, eating behavior and weight loss dynamics are not the same in every patient. Therefore, when describing the mechanism, it is better to think in terms of “possible/intended effect” rather than precise sentences.
Possible effects targeted by fundal ablation
- Supporting appetite reduction: In some patients, earlier satiety and easier portion control are aimed.
- Helping to regulate eating behavior: It is aimed to support behavioral change by strengthening the feeling of satiety, especially in people with frequent snacking or uncontrolled eating tendency.
- Providing “initial support” to the weight loss process: The first period of endoscopic weight loss methods can be critical in terms of motivation and compliance.
Why “alone” may not be enough?
Fundal ablation is a tool in obesity treatment; however, obesity is a multifactorial condition. Sleep, stress, insulin resistance, insulin resistance, emotional eating, physical activity level and eating habits have a significant impact on outcomes. Therefore, in most centers, the procedure is planned together with dietitian follow-up and behavior change programs.
Practical advice: If you are considering “endoscopic weight loss”, ask not only about the procedure but also about the follow-up protocol. questions such as “How many controls are there, what are the diet phases, is there psychological support if needed?” directly affect the likelihood of success.
How is Fundal Ablation Performed? Step-by-Step Process, Recovery and Nutrition
“How is fundal ablation performed?” is one of the most frequently searched topics by patients at the decision stage. Although the protocol may vary from center to center, the general patient journey usually includes the following steps:
1) Preliminary assessment (suitability and safety)
- Body mass index (BMI) assessment
- Blood tests, additional tests deemed necessary
- Review of medications (especially blood thinners)
- Evaluation in terms of stomach diseases such as reflux, gastritis, ulcer
- Analysis of dietary habits and previously tried methods
At this stage, the physician decides whether fundal ablation or another endoscopic obesity treatment option is more suitable for you. (For more information about BMI, please see our BMI calculation guide content)
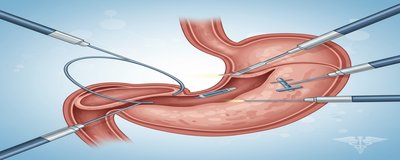
2) Day of procedure: Endoscopic procedure
- The procedure is usually performed in the endoscopy unit.
- The type of sedation/anesthesia is determined by the patient’s condition, the center’s practice and the anesthesia assessment.
- The duration of the procedure may vary depending on the case detail.
There is a short observation period after the procedure, and in many patients, discharge can be planned on the same day (this part depends entirely on clinical judgment).
3) First days Expected complaints
Short duration in some patients:
- Stomach tenderness, cramp-like pain
- Nausea
- Reflux-like complaints may occur. The severity and duration of symptoms vary from person to person. Severe abdominal pain, signs of bleeding, high fever, persistent vomiting require urgent evaluation.
4) Nutrition after fundal ablation (general framework)
Although the nutrition plan varies according to the center, it is mostly gradual:
- Liquid period: Water, sugar-free/appropriate drinks, protein supplements according to physician-dietician recommendation
- Puree-soft period: Small portions that do not tire the stomach
- Graded normal nutrition: Protein-oriented, good fiber and vegetable balance, portion controlled
The critical point here is this: Nutrition after fundal ablation is one of the main factors determining the success of the procedure. instead of the approach of “my appetite will decrease anyway”; planned meals, adequate protein, water consumption and regular follow-up should be targeted. For a detailed sample plan on this subject, you can get support from our nutrition in obesity treatment page.
Who is Suitable for, Who is Not Suitable for? Risks and Comparison with Alternatives
One of the most important topics about fundal ablation is the question “who is fundal ablation applied to?”. Because not every endoscopic method is suitable for every patient profile.
Who may be suitable for fundal ablation?
With physician evaluation, usually:
- People with motivation who have not achieved sufficient results with diet-exercise
- Those who are willing to pursue lifestyle change
- Eligible candidates exploring endoscopic weight loss options and seeking an alternative to surgery
- People who can comply with the regular follow-up (dietitian/physician control) plan
Note: Eligibility is determined not only by weight but also by eating behavior, comorbidities and gastric health.
Who may not be suitable for (Contraindications)
Only a physician can make a definitive list, but in general, more careful evaluation is required in the following cases:
- Conditions such as active stomach ulcer, severe gastritis
- Patients at high risk of bleeding, use of certain blood thinners
- Pregnancy or suspected pregnancy
- Uncontrolled eating disorders and serious psychiatric conditions
- Conditions that may prevent endoscopy/sedation
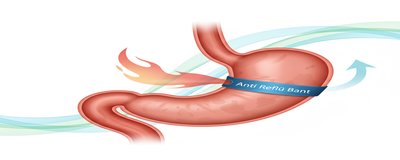
Fundal ablation risks and side effects
Like any medical procedure, fundal ablation has risks. Most common symptoms:
- Nausea, transient stomach pain/sensitivity
- Possibility of increase in reflux complaints (may vary according to the person)
- In rare cases, bleeding, infection or endoscopy-related complications
What is important here is that the procedure is performed by an experienced team, with appropriate patient selection and a strong follow-up plan.
Short comparison with other methods (facilitates decision making)
- Fundal ablation vs gastric balloon: Gastric balloon provides satiety by occupying volume inside the stomach; it is removed after a certain period of time. Fundal ablation targets a different mechanism.
- Fundal ablation vs endoscopic sleeve gastroplasty (ESG/endoscopic gastric reduction): In ESG, the gastric volume is reduced with sutures; usually more pronounced volume restriction is aimed.
- Fundal ablation vs bariatric surgery: Surgical methods are more invasive but may achieve higher and more permanent weight loss in some patients; risk and follow-up dynamics are different.
If you are undecided, you can also take a look at our endoscopic weight loss methods comparison content to see the options on one page.
Frequently Asked Questions (short SEO-oriented answers)
- **The duration of the effect may vary according to the person, follow-up program and lifestyle; long-term data and permanence should be discussed with the physician.
- **“A single number” is not accurate; initial weight, nutritional compliance, activity and metabolic factors determine the outcome.
- **The equipment of the center, anesthesia, hospital conditions, follow-up package and additional examinations may affect the cost.
- **In some patients, reflux complaints may increase or change; those with a history of reflux should be evaluated beforehand.
This content is for informational purposes; diagnosis and treatment require the evaluation of the relevant specialist physician.