What is Gastroenterology Surgery? Which Transactions Are Performed?
Although the words “gastroenterology” and “surgery” are often mentioned together in complaints related to the digestive system, this is precisely the issue that confuses patients the most: what is gastroenterology surgery, in which cases is surgery really necessary and which procedures can be performed with “non-surgical” endoscopic methods? In this article, we will clarify the difference between gastroenterology procedures and gastroenterology surgeries and provide a comprehensive framework from diagnosis to treatment, from endoscopic interventions to laparoscopic (closed) operations.
The general approach in most gastrointestinal diseases is stepwise: first examination and tests, then medication/lifestyle adjustments, endoscopic (internal) treatments if necessary, and finally surgery. Therefore, questions such as “I had an endoscopy, is this surgery?” or “I had ERCP, is it considered surgery?” are very natural. Our aim is to make the terms understandable, to explain which procedure is done for what and to guide you to the right branch (Note: This content is for informational purposes; diagnosis and treatment plan must be determined by physician evaluation)
What is Gastroenterology Surgery? (Gastroenterology or Digestive System Surgery?)
although the expression “Gastroenterology surgery” is commonly used in everyday language, it describes the intersecting aspects of the two fields in medical practice. In short:
- Gastroenterology: A subspecialty of internal medicine. It deals with the diagnosis and medical (drug/lifestyle) treatment of diseases of the stomach, intestines, liver, pancreas and biliary tract. In addition, many gastroenterology procedures such as gastroscopy, colonoscopy, ERCP can be performed by gastroenterology specialists.
- Digestive system surgery (gastrointestinal surgery): It is usually evaluated under General Surgery. It comes into play in cases that require surgery such as reflux surgery, gallbladder surgery, intestinal surgery and oncologic surgery.
Therefore, the practical answer to the question “what is gastroenterology surgery?” is the following: It is the diagnosis and treatment process planned by gastroenterology (endoscopic/medical) and gastrointestinal surgery (surgical) teams together in diseases of the digestive system.
In many centers, the process is multidisciplinary: gastroenterology, general surgery, radiology, pathology, oncology and anesthesia teams can make a joint decision for the same patient. Especially in cases such as bleeding, obstruction, suspicion of tumor, bile duct obstruction, this teamwork both accelerates the correct diagnosis and helps to determine the most appropriate treatment option.
Why is the difference between gastroenterology and general surgery important?
The patient’s response to the question “the difference between gastroenterology and general surgery”, which is frequently searched in SEO, is as follows:
- If the cause of your complaint can be managed with medication/lifestyle, gastroenterology is at the forefront.
- If the problem requires surgery, such as organ removal, repair or resection, gastrointestinal surgery (general surgery) comes into play.
- In some cases (e.g. bile duct stones), endoscopic treatment such as ERCP may be planned first, followed by surgery.
In Which Situations Does Surgery Come to the Agenda? (Symptom-Diagnosis-Treatment Steps)
Not every gastrointestinal complaint results in surgery. In most patients, less invasive methods are tried first. However, in some cases digestive tract surgery may be the most effective option or may be urgently needed.
Emergencies that call for surgery
The following conditions may require urgent evaluation:
- Severe abdominal pain and signs of acute abdomen (e.g. suspected appendicitis)
- Intestinal obstruction (inability to pass gas or stool, vomiting, marked abdominal distension)
- Suspicion of perforation (perforation)
- Active gastrointestinal bleeding that cannot be controlled by endoscopy**
- Intra-abdominal injuries due to trauma (in some cases)
The aim in this table is not to scare, but to answer the question “when should it not be delayed?”. Because early intervention in some complaints both reduces the risk of complications and increases the chance of recovery with a more limited treatment.
Conditions that may require planned (elective) surgery
- Uncontrolled advanced reflux and/or hiatal hernia despite drug treatment
- Gallstones with recurrent attacks or complications gallbladder stones
- Advanced diverticulum disease, recurrent infections or strictures
- Suspicion or diagnosis of gastric/colonic tumor (with surgical oncology planning)
- Stenosis that cannot be opened by endoscopic methods** (stents in some patients, surgical options in some patients)
Why is the step approach important?
Physicians usually start with the “least invasive”. The typical sequence is as follows:
- Examination + blood tests + imaging (USG, MRI, CT etc.)
- Medical treatment and dietary adjustments
- Gastroenterology procedures (diagnostic/therapeutic endoscopic procedures such as gastroscopy, colonoscopy, ERCP)
- gastroenterology surgeries (laparoscopic or open surgery) if necessary
If you want to look at related topics in more detail, you can also review our following contents: What is colonoscopy? and What is ERCP?.
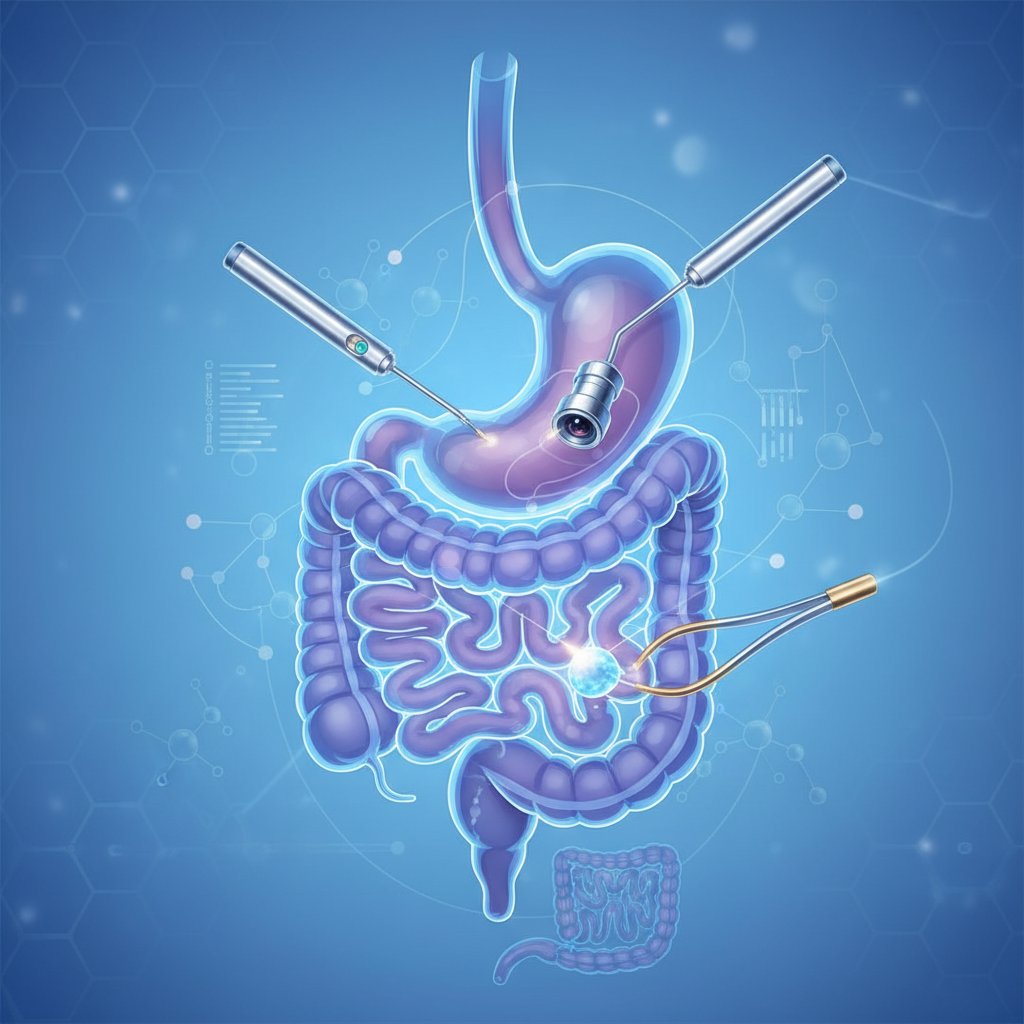
Gastroenterology Procedures: Endoscopic Diagnosis and Treatment Methods
an important part of the question “Which procedures are performed?” covers endoscopic interventions performed without entering the operating room. Although the term “endoscopic surgery” is sometimes used at this point, most procedures are not technically “surgery”; they are diagnostic/treatment applications performed from the inside with an endoscope. However, some endoscopic treatments are advanced and can be an alternative to surgery or complement surgery.
Diagnostic endoscopic procedures
- Gastroscopy: The esophagus, stomach and duodenum are examined. It is used in cases such as reflux, gastritis, ulcer, bleeding focus, suspicion of celiac disease.
- Colonoscopy: It is the examination of the large intestine. It is performed in cases such as anemia, blood in the stool, chronic diarrhea/constipation, colon cancer evaluation for screening purposes.
- Endoscopic ultrasound (EUS): In some centers, it is used to evaluate lesions of the pancreas, biliary tract and digestive tract wall.
Therapeutic endoscopic procedures
- Biopsy collection: Samples are taken from suspicious areas; plays a critical role in clarifying the diagnosis.
- Polypectomy (polyp removal): Removing polyps during colonoscopy can reduce the risk of colon cancer. Patients often ask “did I have surgery?”; most of the time this procedure is an endoscopic treatment.
- Stop bleeding: Clip, injection or burning methods can be applied with endoscopy.
- **Gap widening and stenting: If there is stenosis in areas such as the esophagus/colon, balloon dilatation or stenting can be applied.
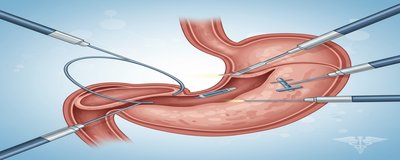
- ERCP: It is an advanced procedure used in the treatment of stones, stenosis or obstructions in the bile and pancreatic ducts (applications such as stone removal, sphincterotomy, stenting).
These procedures are often performed under sedation (sleep state) and depending on the patient’s condition, discharge may be possible on the same day. Nevertheless, since each procedure has risks and preparation requirements, the physician’s recommendations should be followed exactly. For more information: you can take a look at our articles What is endoscopy? and What is gastroscopy?.
Mini guide: “Is an endoscopic procedure surgery?”
- Diagnostic endoscopy (imaging only + biopsy): It is usually not considered surgery.
- Therapeutic endoscopy (polyp removal, stopping bleeding, stents, etc.): It is therapeutic; however, it is often not classified as “surgery”.
- Surgery: It is an open/laparoscopic surgical intervention for intra-abdominal organs.
Gastroenterology Surgeries: Common Operations in Digestive System Surgery
Gastroenterology surgeries refer to operations performed within the scope of “gastrointestinal surgery”. These operations can be performed with open surgery or laparoscopic (closed) methods, which are more preferred today. Which technique to choose depends on the type and extent of the disease, the general condition of the patient and the surgeon’s assessment.
Upper gastrointestinal tract surgery
- Reflux surgery (fundoplication): It can be considered in patients whose complaints persist despite medication, complications develop or anatomical problems (such as hiatal hernia) are detected.
- Hiatal hernia (stomach hernia) surgery: In cases where part of the stomach slides up the diaphragm, surgery may be considered if the symptoms are severe. (Related content: To whom is reflux surgery performed?)
Gallbladder and biliary tract
- Laparoscopic cholecystectomy (gallbladder surgery): May be recommended if gallstones cause recurrent attacks, inflammation or risk of pancreatitis. For specific guidance: Gallbladder surgery.
Small bowel and colon surgery
- Appendicitis surgery: One of the most common emergency surgeries; can be performed laparoscopically in most cases.
- Diverticulitis surgery: May be considered if recurrent attacks, complications (abscess, fistula) or stricture develop.
- Colon resections: It may be necessary in cases of tumors, advanced polyp disease, stenosis or some inflammatory bowel diseases (e.g. cases with complications).
Is “endoscopic surgery” the same as laparoscopic surgery?
Answer. This is where the confusion is most common:
- Endoscopic procedures: Interventions performed through the digestive canal by entering through the mouth or anus.
- Laparoscopic surgery: It is a “closed surgery” in which small incisions are made through the abdominal wall to target organs inside the abdomen.
Both approaches can be minimally invasive, but the targeted area, the devices used and the extent of treatment are different.
Pre-Procedure/Pre-Operative Preparation, Risks and Recovery: What Should Patients Pay Attention To?
Whether endoscopic intervention or surgery is planned, preparation and follow-up are essential for a safe process. The following articles are for general information purposes; your personal plan should be determined by your physician.
Frequently requested preparations before the procedure
- Hunger duration: You are usually asked to fast for a certain number of hours during endoscopy and surgery.
- Medication regulation: Especially blood thinners (aspirin, clopidogrel, warfarin, etc.) and some diabetes medications may affect the procedure plan. Never stop the medication on your own; physician guidance is essential.
- Bowel cleansing: Preparation before colonoscopy is critical for image quality.
- Examinations: Evaluations such as blood tests, ECG, chest radiography may be required.
Potential risks (general framework)
As with any medical intervention, there may be risks such as sedation-related side effects, bleeding, infection, and rarely perforation. In addition to these, risks related to anesthesia and complications related to the recovery process are also evaluated in surgery. Your doctor should clearly explain the risk-benefit balance for you.
Practical advice for the healing process
- Follow the post-discharge feeding plan; gradual feeding may be recommended after some operations.
- Note any pain, fever, nausea, vomiting or changes in stool.
- Keep your follow-up appointments; the follow-up plan is particularly important for endoscopic procedures with expected pathology results.
When to contact the emergency room?
If you have the following symptoms, contact your healthcare provider without delay:
- Severe/increased abdominal pain
- Bloody vomit or black tarry stools
- High fever, chills
- Jaundice (marked yellowing of the eyes/skin)
- Fainting, severe weakness, rapid pulse
Frequently Asked Questions (FAQ)
Which department is gastroenterology surgery?
In cases requiring surgery, General Surgery (gastrointestinal/digestive system surgery) is usually involved. Gastroenterology is involved in endoscopic diagnosis/treatment and medical management. In many cases the two branches work together.
Is endoscopy surgery?
In most cases, no. Endoscopy can be a diagnostic or therapeutic procedure, such as polyp removal/stopping bleeding, but it is not “surgery” in the classical sense.
What does it mean to remove polyps during colonoscopy?
Endoscopic removal of polyps detected during colonoscopy (polypectomy). The follow-up interval and the plan for the next colonoscopy are determined according to the pathology result.
Is ERCP risky?
ERCP is an advanced gastroenterology procedure and has risks like any other procedure; however, when performed by an experienced team with the right indication, the benefit can be high. Risk assessment is patient-specific.
Correct diagnosis and selection of the right method in digestive system complaints allows avoiding unnecessary procedures and, when necessary, receiving the most effective treatment in a timely manner. if you think you need an evaluation within the scope of “Gastroenterology surgery”, you can create a personalized roadmap by sharing your complaints and previous examinations, if any, with a specialist.