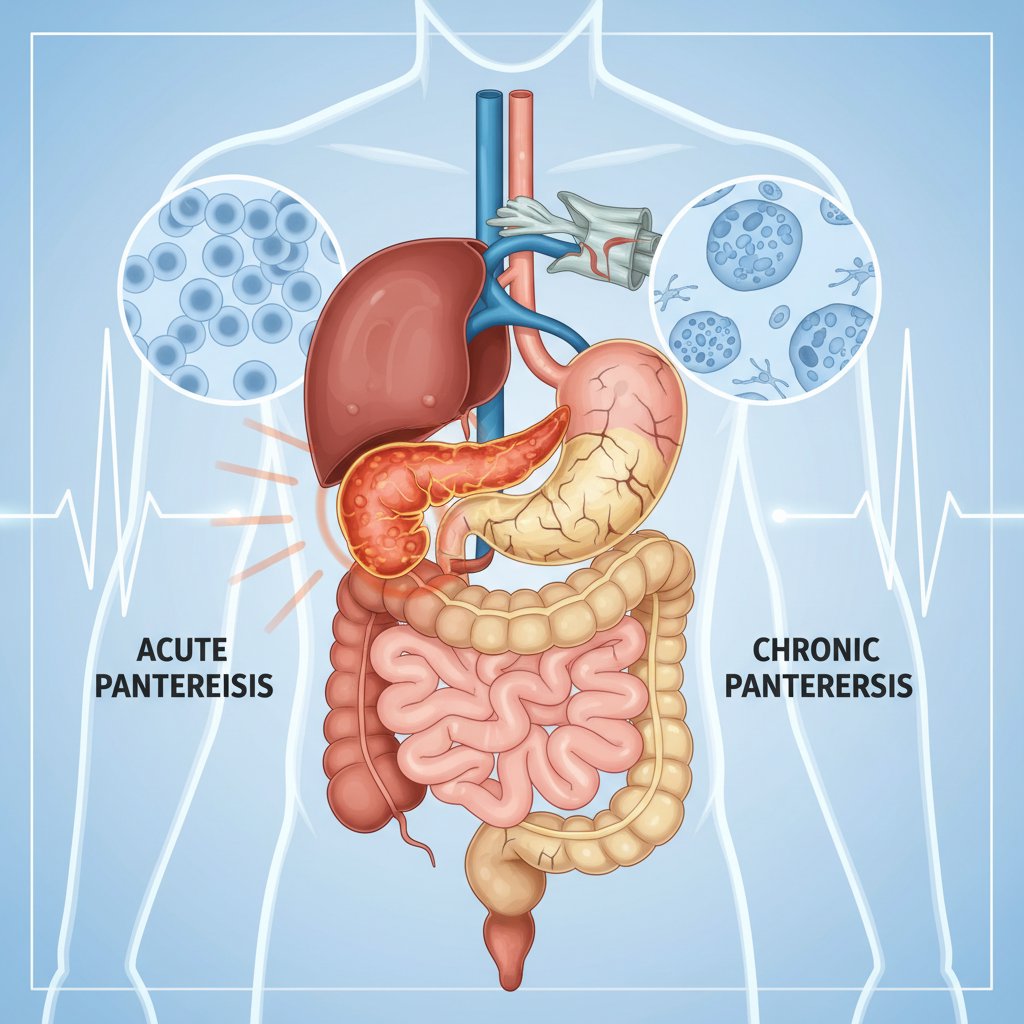
What is Pancreatitis? Symptoms of Acute and Chronic Pancreatitis (Guide to Pancreatic Inflammation)
Pancreatitis, or pancreatitis, is an inflammation of the pancreas, which produces vital enzymes for digestion and hormones that regulate blood sugar. It most commonly occurs in two forms: *acute pancreatitis (sudden onset, often resolving with the right treatment) and chronic pancreatitis (recurrent/long-lasting, which can leave permanent damage to the pancreas over time). the question “What is pancreatitis?” usually comes up when investigating severe abdominal pain, nausea and vomiting or “symptoms of pancreatitis”.
In this article you will find a user-friendly yet comprehensive guide to acute and chronic pancreatitis symptoms, what pancreatitis pain looks like, what causes pancreatitis, the diagnostic process and treatment of pancreatitis. We have also included warning signs that clearly answer the question “when is pancreatitis an emergency?”.
Note: This content is for informational purposes only. If you have severe abdominal pain, fever, jaundice or persistent vomiting, seek medical attention without delay.
What is pancreatitis (inflammation of the pancreas) and how does it develop?
The pancreas is an organ located behind the stomach and has two main functions:
- Digestive enzymes (help break down fats, proteins and carbohydrates)
- Hormones (regulate blood sugar, especially insulin and glucagon)
Pancreatitis is associated with digestive enzymes produced by the pancreas that are prematurely activated in the pancreas when they should normally be activated in the intestine and “irritate and inflame” the tissue. This can cause pain, nausea, vomiting and in some cases serious systemic effects (low blood pressure, organ involvement).
While pancreatitis sometimes progresses as a one-time attack (acute), sometimes chronic pancreatitis may develop as a result of repeated damage. In particular, factors such as alcohol use, smoking, gallstones and high triglycerides can increase the risk of pancreatitis.
A frequently asked question at this point is: **Yes; if the underlying cause is not corrected (e.g. gallstones, alcohol, very high triglycerides), attacks may recur and the risk of chronicity increases over time.
What is Acute Pancreatitis? Symptoms of Acute Pancreatitis and “Where Does the Pain Hit?”
Acute pancreatitis is a sudden onset of inflammation of the pancreas. It may have a mild course, or in some cases it may become severe and require close follow-up in the hospital. One of the most searched topics by users is “symptoms of acute pancreatitis “ and “where does pancreatitis pain hit? “.
Symptoms of acute pancreatitis (most common)
- Severe pain in the upper abdomen (epigastric): It usually starts suddenly.
- Pancreatitis pain may radiate to the back: “Girdle-like” or radiating pain to the back is typical. It can therefore be confused with “pancreatic pain”.
- Nausea and vomiting: Especially with pain, sometimes recurrent.
- Fever: It does not always occur but may be seen with infection/inflammatory response. the answer to the question “Does pancreatitis cause fever?” is: in some cases, yes.
- Sensitivity and bloating in the abdomen
- **Loss of appetite, weakness
- Jaundice (in some patients): In gallstone-induced pancreatitis, yellowing of the eyes/skin may be seen due to bile duct involvement.
“When to go to the emergency room?” (red flags)
The answer to the question when pancreatitis is urgent is clear in the following situations: **Urgent evaluation is required without waiting
- Intolerable/increased abdominal pain
- Constant vomiting, inability to drink fluids
- High fever, chills
- Jaundice, dark urine
- Fainting, confusion
- Shortness of breath, palpitations, marked weakness
What causes acute pancreatitis?
The most common causes are:
- Gallstone pancreatitis: Gallstones can block the bile duct and affect the pancreatic duct.
- Alcohol use: The risk increases especially with heavy/long-term use.
- High triglyceride levels can trigger pancreatitis: Very high triglyceride levels can trigger pancreatitis.
- Some medications, after ERCP, infections and more rarely autoimmune causes.
Tip: For the subject of “lipase”, which is frequently mentioned in blood tests, you can take a look at our article **[What does lipase elevation mean?
What is Chronic Pancreatitis? Chronic Pancreatitis Symptoms, Complications and Nutrition
Chronic pancreatitis is a condition characterized by permanent damage and loss of function of the pancreas over time. It may develop as acute attacks recur or long-term risk factors persist. The search intention here is often centered around “symptoms of chronic pancreatitis”, “nutrition in chronic pancreatitis” and “treatment of pancreatitis**”.
Symptoms of chronic pancreatitis
- Recurrent or persistent upper abdominal pain: In some people, the pain may decrease over time; this may be associated with increasing loss of pancreatic function, not improvement.
- Weight loss: May be due to loss of appetite and malabsorption.
- Fatty, foul-smelling stools (steatorrhea): When pancreatic enzymes are reduced, fat digestion is impaired.
- Bloating, gas, diarrhea
- Blood sugar irregularity / diabetes: “Does chronic pancreatitis cause diabetes?” Yes, diabetes can develop if the hormone production of the pancreas is affected.
Complications in chronic pancreatitis
- Malabsorption (malabsorption) and related vitamin/mineral deficiencies (especially fat-soluble vitamins)
- cystic formations such as pancreatic pseudocyst
- Decreased quality of life due to pain, malnutrition
- Development of diabetes
Causes and risk factors for chronic pancreatitis
- alcohol and smoke (together the risk increases even more)
- Genetic predisposition (in some cases)
- More rare causes such as autoimmune pancreatitis
Chronic pancreatitis nutrition (practical advice)
Depending on the individual, the most commonly recommended approach is:
- Alcohol should be completely quit, smoking should be quit
- facilitating digestion with small and frequent meals
- Physician/dietitian plan for fat consumption (some patients may require controlled fat + enzyme therapy)
- pancreatic enzyme replacement when necessary (on doctor’s recommendation)
- Monitoring vitamin/mineral levels
Tip: Prolonged abdominal pain can be caused by different reasons. For similar complaints, you can also review our Causes of abdominal pain content.
Differences Between Acute and Chronic Pancreatitis + Overview of Diagnosis and Treatment
Differentiating between acute and chronic is important for proper management. The summary below allows you to quickly see the main differences between “symptoms of acute and chronic pancreatitis”:
Acute vs. Chronic pancreatitis (brief comparison)
- Onset: Acute starts suddenly; chronic develops over a longer period.
- Pain: Severe and sudden in acute; may be recurrent or persistent in chronic.
- Digestive problems: More nausea-vomiting in acute; steatorrhea, weight loss, bloating may be more prominent in chronic.
- Permanent damage: In acute there is not always permanent damage; in chronic there is a high risk of loss of pancreatic function.
How is pancreatitis diagnosed?
A doctor’s evaluation usually includes the following steps:
- Blood tests: especially lipase elevation and/or amylase increase (not always necessary).
- Imaging: Methods such as ultrasound (especially for gallstones), CT or MR/MRCP.
- Cause investigation: Gallstones, triglycerides, alcohol history, medications, etc.
Treatment of pancreatitis (general approach)
Treatment depends on the severity and cause of pancreatitis:
- Treatment of acute pancreatitis: Fluid support, pain control, nutrition plan and management of the underlying cause (e.g. gallstones).
- Treatment of chronic pancreatitis: Pain management, nutritional support, enzyme replacement, vitamin monitoring; endoscopic or surgical options in some cases.
Important: There is no single answer to the question “How many days does pancreatitis go away?”. Mild acute attacks may resolve within days; severe cases may require longer hospitalization. Chronic pancreatitis may require long-term follow-up.
Frequently Asked Questions (FAQ)
Is pancreatitis fatal?
Mild acute pancreatitis often proceeds well, but severe acute pancreatitis can lead to serious complications. This is why urgent evaluation is important in severe symptoms.
Does pancreatitis recur?
Yes. The risk of recurrence increases especially if causes such as gallstones, alcohol use and high triglycerides are not controlled.
Is pancreatitis the same as pancreatic cancer?
No, they are not. Pancreatitis and pancreatic cancer are different diseases. However, a physician’s assessment is essential for long-term complaints.
Sources and Medical Note
- American College of Gastroenterology (ACG) clinical approaches
- NHS (UK) patient information pages
- Mayo Clinic patient guides
Final note: This article provides general information; diagnosis and treatment require evaluation by a gastroenterologist or general surgeon. If you have severe abdominal pain, jaundice, fever or persistent vomiting, contact the emergency room without delay.