What is Reflux Disease? Gastroesophageal Reflux (GERD) Symptoms and Treatment
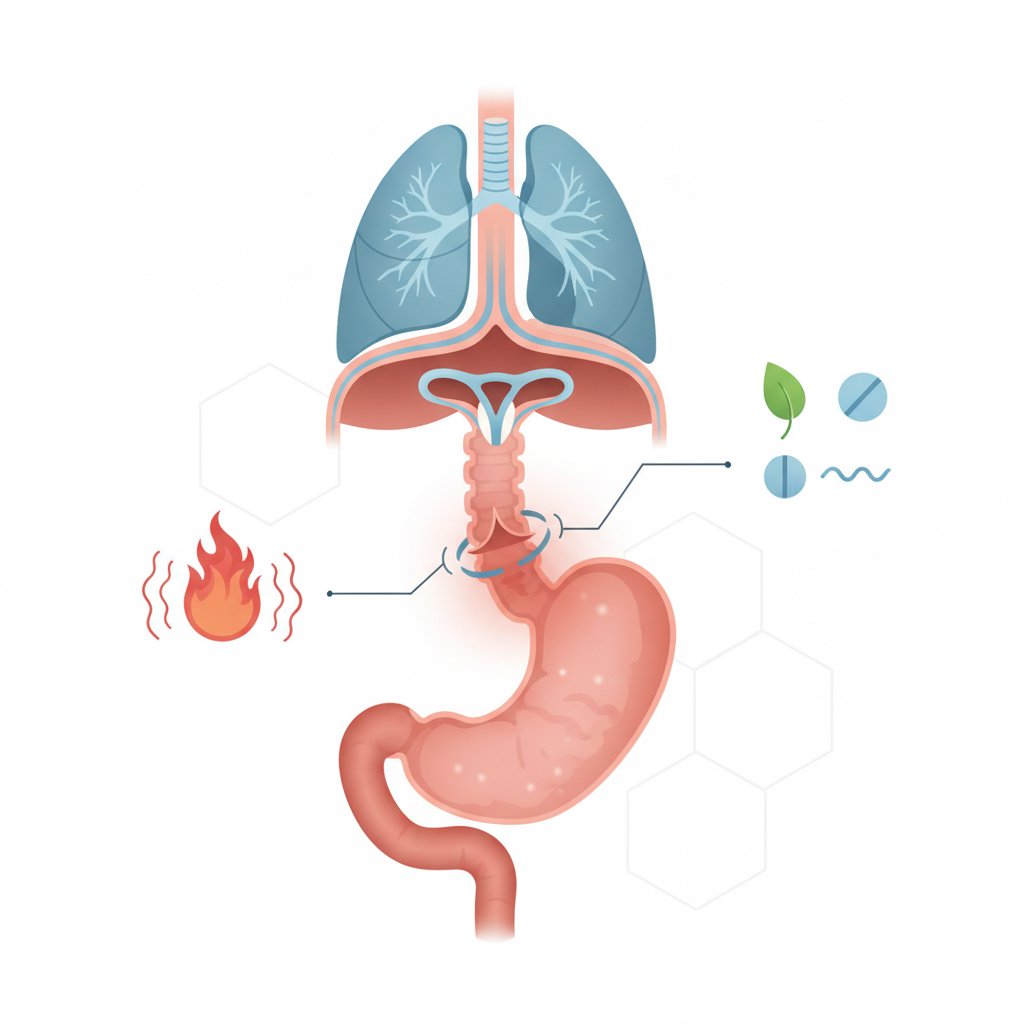
Reflux is a very common digestive system problem, popularly known as “stomach acid escaping upwards”. However, not every heartburn complaint means “reflux disease”. **The most accurate answer to the question “What is reflux? It is the escape of stomach contents (acid, enzymes and sometimes bile) back into the esophagus. If this backflow occurs occasionally, it can be considered “physiological reflux”; but if the complaints become frequent, reduce the quality of life or cause damage to the esophagus, gastroesophageal reflux disease (GERD) comes to the fore.
In this article, we will discuss frequently wondered topics such as reflux symptoms, reflux causes, night reflux, silent reflux (LPR), as well as how to diagnose reflux and reflux treatment steps in a detailed and understandable way. If you are looking for information on reflux in children/infants, you will also find references to the content we have prepared. (Example: Nutrition and Swallowing Development in Children and Reflux Guide in Babies
What is Reflux? When is Reflux Disease (GERD) Called?
Gastroesophageal reflux is when the lower esophageal sphincter (LES), which acts as a valve between the stomach and esophagus, does not close tightly enough and stomach contents escape upwards. This may increase especially after meals, with bending/reclining or at night. Reflux disease is defined not only by “acid escape” but also by the fact that this escape causes complications such as symptoms, frequent recurrence and/or irritation of the esophagus (esophagitis).
To make a practical distinction:
- If you experience occasional heartburn and are relieved by lifestyle adjustments, this may be physiologic reflux.
- If symptoms occur more than 2 times a week, wake you up at night, cause difficulty swallowing or persist for a long time, you may need to be evaluated for GERD.
Reflux can occur in all age groups. Although it is more frequently discussed in adults, searches for reflux symptoms in children and especially reflux symptoms in infants are quite common. Although similar mechanisms play a role in the pediatric period, the evaluation and approach varies according to age. Therefore, it is important to consult the pediatrician and, if necessary, pediatric gastroenterology if there is suspicion in children.
Why Does Reflux Happen? Risk Factors and Triggers
the answer to the question “Why does reflux happen?” is usually not reducible to a single cause. The most common mechanism is relaxation of the EDS or increased gastric pressure. The following conditions may increase the risk of gastroesophageal reflux:
Common risk factors
- Overweight / increased intra-abdominal pressure: As the pressure in the abdominal area increases, it becomes easier for the stomach contents to escape upwards.
- Hiatal hernia (gastric hernia): If part of the stomach slides up from the diaphragm, it may impair the function of the ACS. (High search intent: hiatal hernia reflux.)
- Pregnancy: Especially in the last trimester, reflux may become more frequent with increased pressure and hormonal effects (reflux in pregnancy).
- Smoking and alcohol: May decrease sphincter pressure and increase irritation.
- Eating late: It is an important trigger especially for night reflux.
- Some medications: Medications such as some painkillers, muscle relaxants or certain blood pressure medications can increase reflux. (Always consult a doctor for medication changes)
Nutritional triggers: personalization instead of a “forbidden list”
There is often a “reflux diet forbidden list” circulating on the internet; however, the most accurate approach is to identify individualized triggers. For some people, tomatoes, chocolate, coffee, spices, peppermint, fried/fatty foods, carbonated drinks may increase the symptoms; for others, they may not. Best practice:
- keep a nutrition and symptom diary for 1-2 weeks,
- Recognizing the foods that increase the complaint and adjusting the portion/frequency,
- it means trying to eat “little and often”.
This personalization approach is particularly in line with the user intent behind the search “what is good for reflux”: Not a single list for everyone, but a workable plan.
What are the Symptoms of Reflux? Typical, Atypical (Silent) and Nocturnal Symptoms
Symptoms of reflux may vary from person to person. While some people have classic heartburn, others may have a more “silent” course. It is therefore useful to think of the symptoms under three headings.
1) Typical reflux symptoms
- Heartburn: Burning sensation behind the breastbone; usually increases after a meal.
- Bitter/sour water coming into the mouth (regurgitation): May be especially pronounced when bending or lying down.
- Burning/pressure in the chest: Sometimes it can be confused with pain originating from the heart. If chest pain is severe or accompanied by shortness of breath, urgent evaluation may be required.
2) Atypical symptoms: “silent reflux (LPR)” / throat reflux
In some people, reflux may affect more the throat and airways, with no obvious heartburn. This is also known as laryngopharyngeal reflux (LPR). Common atypical symptoms:
- Chronic cough (one of the most common causes of *does reflux cause cough?)
- ** hoarseness** (* hoarseness reflux*)
- Need to clear throat, burning in the throat
- **Sticking sensation in the throat (globus)
- Mouth odor may be associated with reflux
- Enamel erosion (due to acid contact)
Since these symptoms can also be confused with conditions such as allergies, sinusitis, infection or asthma, it is important to be evaluated by a physician if they persist for a long time.
3) Symptoms of night reflux
Night reflux refers to reflux complaints that increase especially when lying down. The following may occur
- Burning that wakes you from sleep
- Acid in the throat, feeling of suffocation
- Sore throat or bad taste in the mouth in the morning
- Night cough
Lifestyle adjustments (meal times, sleeping position) often make a significant difference in people with nocturnal reflux.
How to Diagnose Reflux and How to Treat Reflux (Stepwise Approach)
Diagnosis and treatment of suspected reflux is usually “stepwise”. In other words, simpler and safer steps are tried first, and if necessary, further tests and treatments are carried out.
When to consult a doctor (alarm symptoms)
In the following cases, it is necessary to consult a doctor without saying “wait and it will pass”:
- **Difficulty swallowing (dysphagia), increased sensation of getting stuck
- Involuntary weight loss
- bleeding symptoms such as anemia, black stools, blood in vomit
- Complaints persist and wake you up at night
- new-onset reflux complaints over 50 years of age
- Additional risks such as family history of gastroesophageal cancer
Methods used in the diagnosis of reflux
- Clinical evaluation: Type of complaints, frequency, triggers and lifestyle.
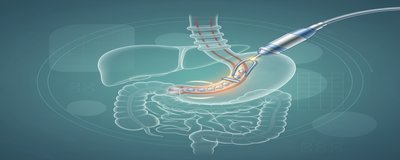
- Endoscopy: Endoscopy may be requested especially if there are alarm signs, prolonged complaints or non-response to treatment. Endoscopy shows conditions such as esophagitis, ulcer, stenosis (endoscopy reflux).
- 24 hour pH meter / pH-impedance: Measures acid escape into the esophagus and its relation with complaints (24 hour pH meter).
- Esophageal manometry: Evaluates esophageal movements and sphincter pressure; may be especially important if surgery is planned.
Treatment of reflux: Lifestyle + nutrition + medication (when needed)
for most people, Treatment of reflux starts with lifestyle steps:
1) Lifestyle changes (most effective practices)
- Finish eating at least 2-3 hours before bedtime (how many hours before bedtime for reflux).
- Small and frequent meals instead of large portions.
- In overweight, weight management with physician recommendation.
- Raising the head of the bed: Not just an extra pillow; if possible, raise the head of the bed by 10-15 cm.
- Do not lie down immediately after a meal; a short walk may be good.
- Avoiding tight belts/clothes.
- Reducing/stopping smoking and alcohol.
2) Medication (as directed by a doctor)
Depending on the severity of the complaint, the physician may recommend medications such as antacid/alginate, H2 blocker or proton pump inhibitor (PPI). The important point here:
- The choice of medication, dose and duration of use should be individualized (this is why the search how long to take reflux medication is very common).
- Regular follow-up rather than prolonged or uncontrolled use is the safest approach.
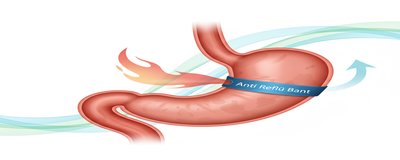
3) Advanced treatments
If complaints persist despite medication, if there is a structural problem such as hiatal hernia or if complications develop, endoscopic/surgical options may be considered (reflux surgery). This decision should be evaluated by gastroenterology and the relevant surgical team.
What’s Good for Reflux? 10 Actionable Tips for Home (For Everyday Life)
let’s answer the question “What is good for reflux at home?” with safe and practical suggestions. The following steps help to reduce symptoms in most people:
- Eat dinner earlier; aim to finish 3 hours before bedtime.
- Reduce fatty/fried meals; eat lighter, especially in the evening.
- Observe potential triggers such as coffee, chocolate, tomatoes, bitter spices; try to reduce them rather than ban them completely.
- Do not lie down immediately after a meal; try a light walk for 10-20 minutes.
- if you have night reflux, raise the head of the bed and try sleeping on your left side (for some people this can be a relief).
- Limit fizzy drinks and late-night snacks.
- Do not eat too fast; chew well and make the bites smaller.
- Practice stress management (breathing exercises, regular sleep). answer to the question “Does stress cause reflux?” Indirectly, yes, stress can increase sensitivity and disrupt eating patterns.
- Make a note of your complaints and what you eat; this will also help with the diagnosis at the doctor’s appointment.
- In case of prolonged, recurrent or alarming symptoms, consult a physician.
As the approach can be different if reflux is suspected in children or babies, you can take a look at our separate resources for parents: Reflux Symptoms in Babies and When to See a Doctor and Eating Problems in Children.
This content is for informational purposes only and is not a substitute for a medical evaluation for diagnosis and treatment.